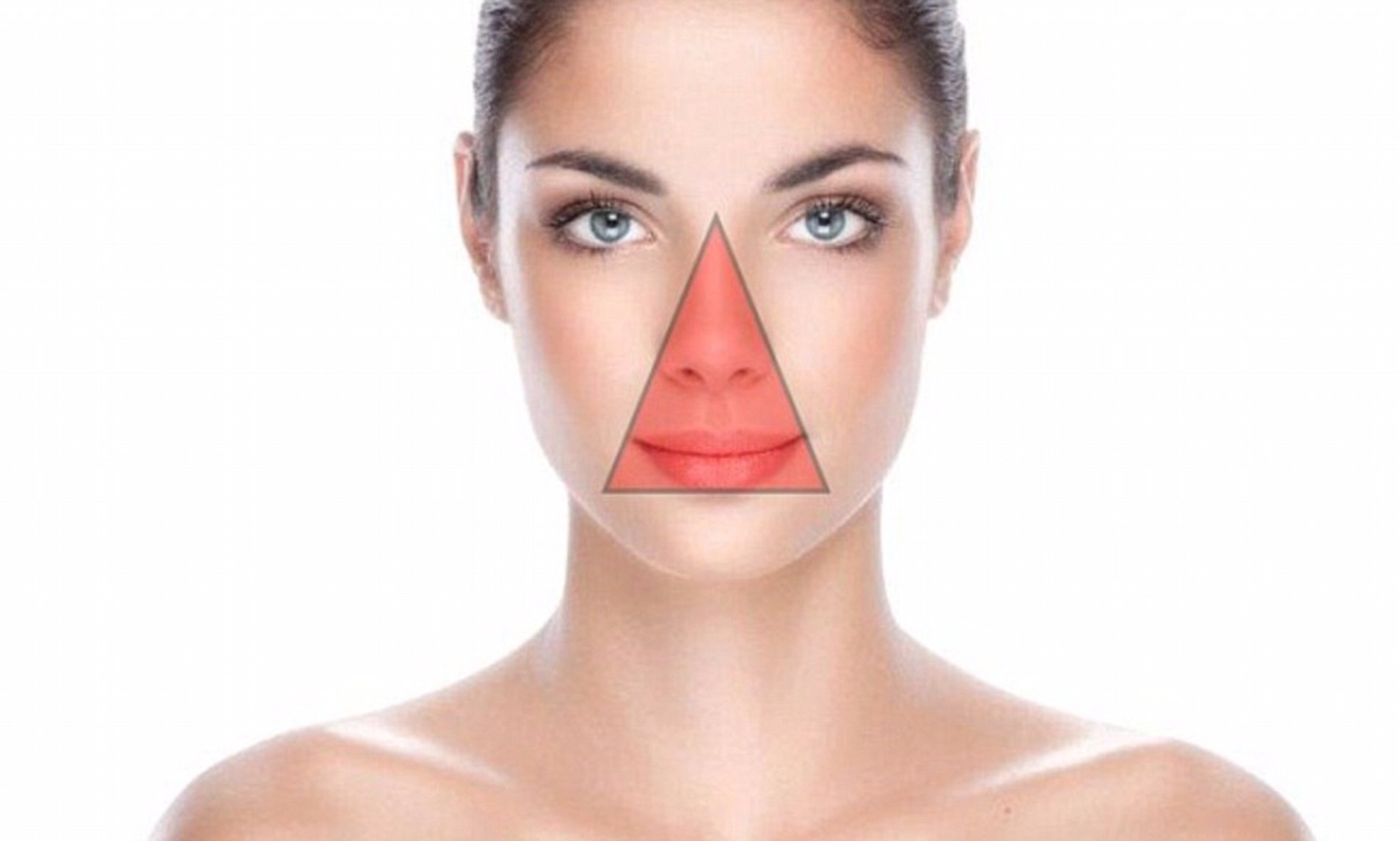
The area between the bridge of the nose and the corners of the mouth, known as the “danger triangle” or “triangle of death,” is often cited as a high-risk zone for popping pimples due to potential complications. Although infections leading to severe outcomes in this region are extremely rare, dermatologists say increased caution around pimple popping is beneficial. This warning stems from the specific anatomy of the danger triangle, where blood vessels connect directly to structures near the brain, theoretically allowing infections to spread more easily.
The central face’s dense network of blood vessels drains into the cavernous sinus, a hollow area near the brain, making it vulnerable to severe infections. In rare cases, a bacterial infection from this region could lead to a life-threatening condition called cavernous sinus thrombosis, where blood clots travel to the brain. Despite these risks, experts clarify that the likelihood of a pimple-popping-induced infection spreading to this degree is very low. Most minor infections are quickly managed by immune cells in the skin, which contain bacteria before they spread.
Invasive procedures in the danger triangle require careful technique to avoid bleeding and blood clots, according to dermatologists. However, in their combined decades of experience, they report almost no cases of serious sinus infections resulting from pimple popping. While there is a slight risk of infection and potential tissue damage, the actual threat of death or severe complications is exceptionally uncommon. Dermatologists still advise against popping pimples in this area to prevent minor issues that could develop.
Popping any pimple, not just those in the danger triangle can lead to unwanted effects, including infection, discoloration, and scarring. Dermatologists emphasize that it’s generally safer to avoid popping pimples entirely. Common pimples include open comedones (blackheads) and closed comedones (whiteheads); the latter are more prone to causing redness and swelling if aggravated. Picking at closed comedones, particularly inflammatory acne, can worsen the appearance and spread bacteria deeper, potentially leading to scarring or pigmentation issues.
For managing pimples without picking, experts recommend using hydrocolloid bandages, or pimple patches, which keep the area protected and reduce the urge to touch the skin. For persistent or stubborn acne, seeing a dermatologist for professional extractions or treatments is a safer approach. Dermatologists agree that patience and proper skin care are more effective and less risky than trying to self-manage acne by popping pimples.
If popping a pimple is unavoidable, dermatologists advise treating it like a minor surgical procedure. This means using clean hands, disinfecting any tools, and applying gentle pressure only if the pimple has come to a head. Over-the-counter treatments such as salicylic acid, benzoyl peroxide, and retinoids are recommended for regular acne management. In cases of severe or cystic acne, seeking professional care early can help prevent long-term damage like scarring and skin discoloration.
