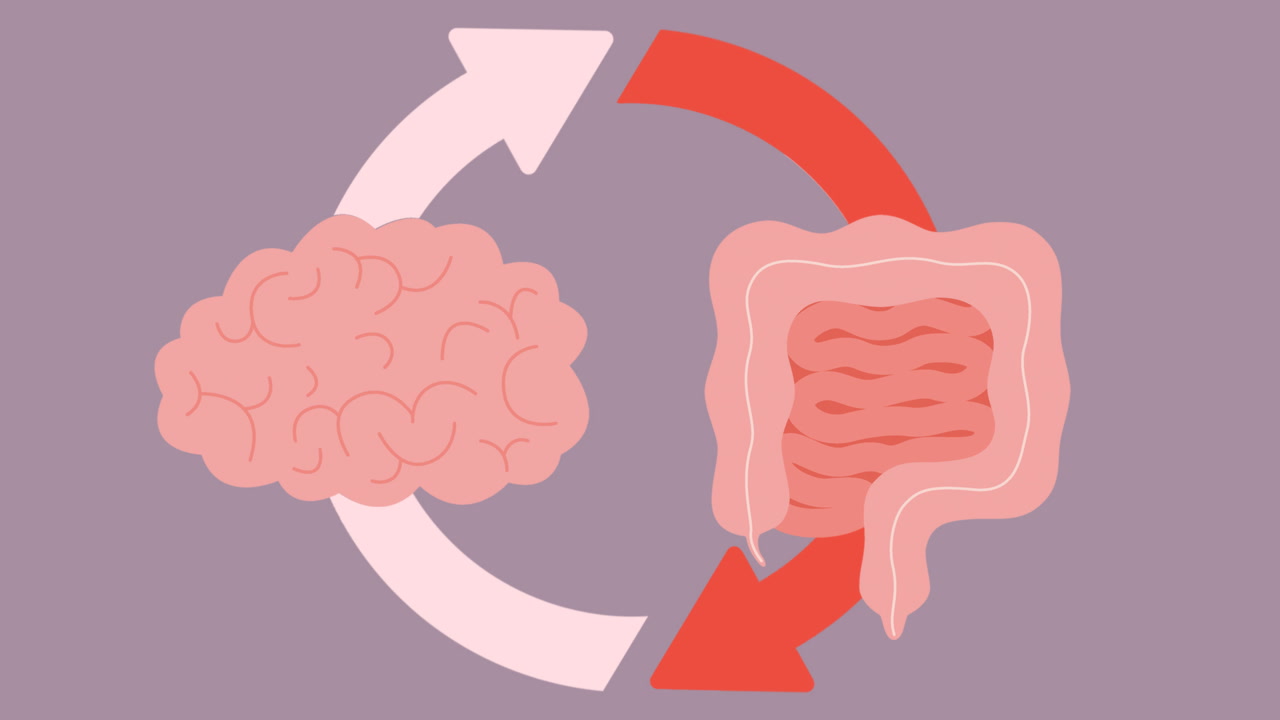
The relationship between what happens in your gut and how you feel mentally is far more profound than most people realize. For decades, medical professionals viewed digestive issues and mental health conditions as separate concerns, but groundbreaking research has revealed an intricate communication network known as the gut-brain axis.
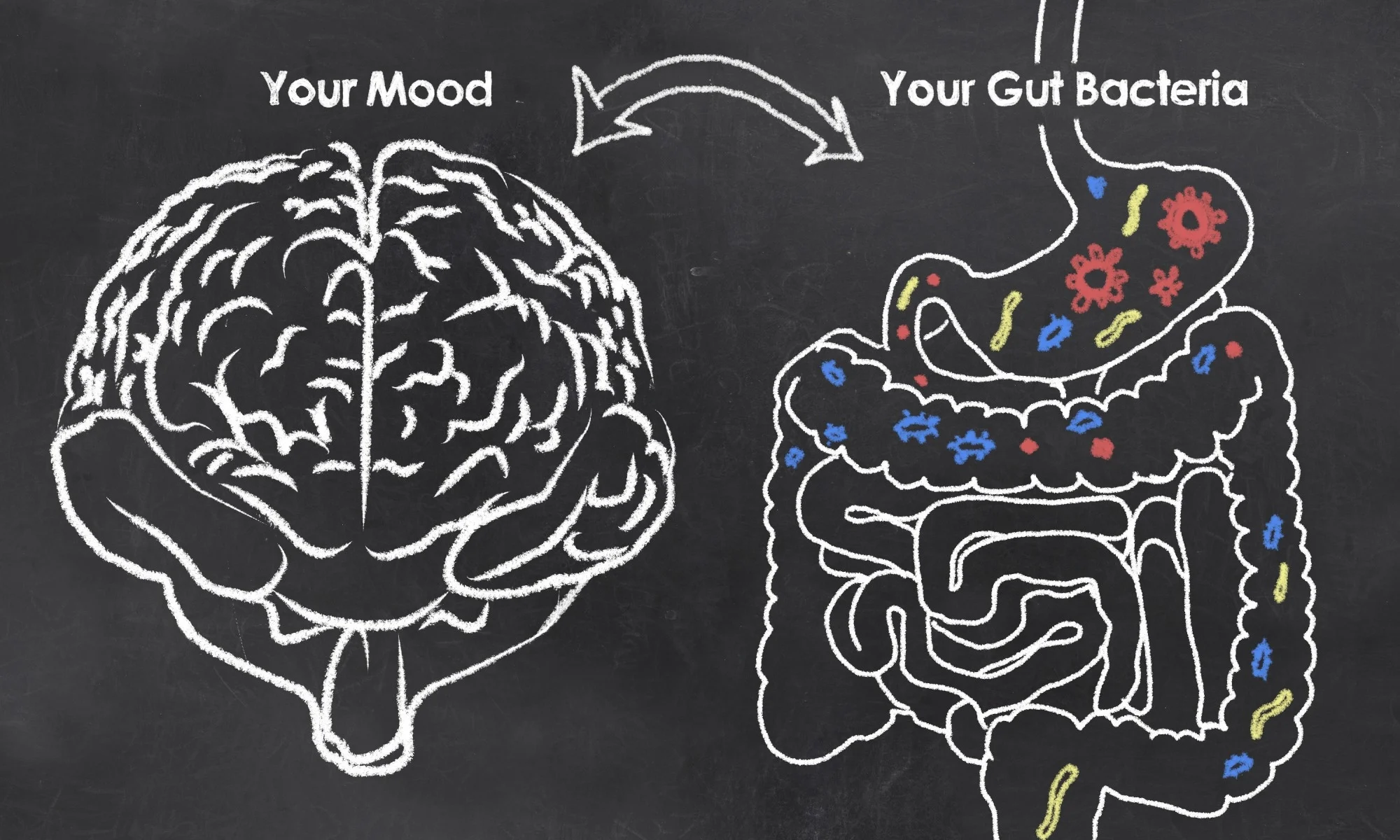
This bidirectional pathway demonstrates that your gut microbiome—the trillions of bacteria, fungi, and other microorganisms living in your digestive tract—plays a crucial role in regulating mood, anxiety, and depression.
Recent studies have shown that people with depression often exhibit significantly different gut microbiome profiles compared to healthy individuals, with certain beneficial bacteria species notably absent. The implications are staggering: approximately 90% of serotonin, the neurotransmitter most associated with mood regulation, is produced in your gut rather than your brain.
This means that the health of your digestive system directly influences your mental state through complex biochemical pathways involving inflammation, neurotransmitter production, and immune system function.
Understanding this connection opens up revolutionary possibilities for treating depression and anxiety through gut-focused interventions. Rather than viewing mental health solely through the lens of brain chemistry, we can now explore how dietary changes, probiotic supplementation, and lifestyle modifications that support gut health might serve as powerful tools for improving mental well-being. This emerging field, known as nutritional psychiatry, represents a paradigm shift in how we approach mental health treatment.
Understanding the Gut-Brain Axis
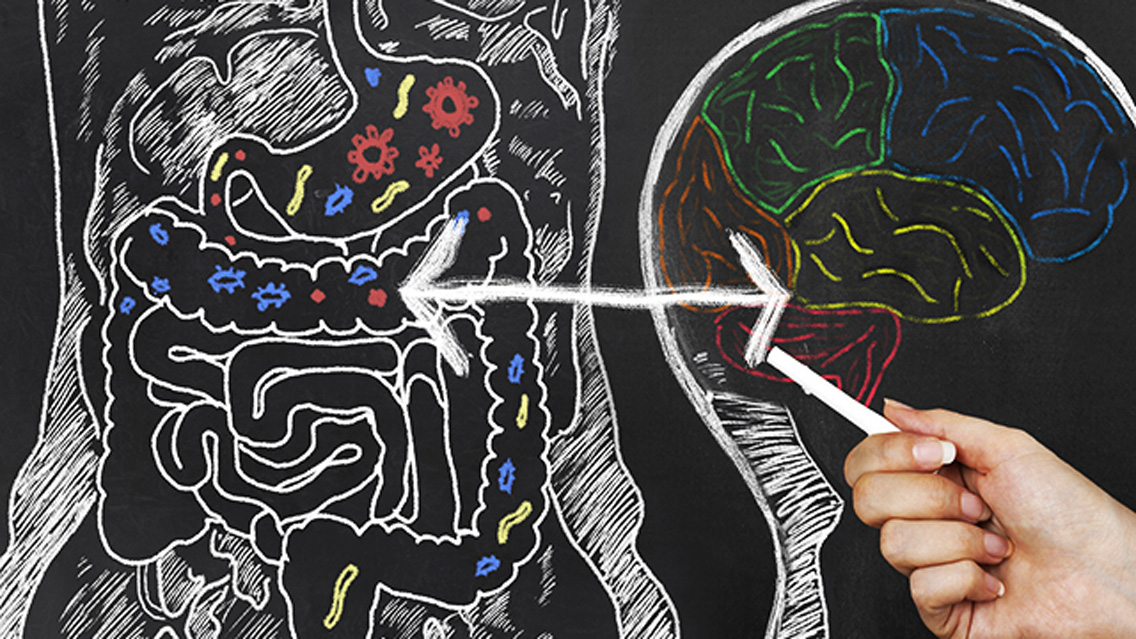
The gut-brain axis represents a sophisticated communication network that connects your central nervous system with your enteric nervous system, often called the “second brain” in your gut. This bidirectional pathway operates through multiple channels, including the vagus nerve, hormonal signaling, and immune system messengers called cytokines.
Your gut microbiota plays a central role in this communication system by producing neurotransmitters and other bioactive compounds that directly influence brain function. When gut bacteria are balanced and diverse, they support healthy neurotransmitter production and maintain proper inflammatory responses. However, when this delicate ecosystem becomes disrupted—a condition called dysbiosis—it can trigger a cascade of negative effects on mental health.
The vagus nerve acts as a primary communication highway between your gut and brain, transmitting both chemical and emotional signals in both directions. When your gut experiences inflammation or bacterial imbalance, these stress signals travel directly to your brain, potentially triggering symptoms of depression, anxiety, or cognitive dysfunction.
The Science Behind Gut Dysbiosis and Depression
Research has consistently demonstrated that people with depression exhibit distinct patterns of gut microbiome disruption. Specific bacterial strains associated with mental health include reduced levels of beneficial bacteria like Coprococcus, Subdoligranulum, and various Ruminococcaceae family members in individuals with depression.
Conversely, harmful bacterial metabolites can compromise the integrity of the blood-brain barrier and increase production of neurotoxic compounds. For example, elevated levels of p-cresol and 4-ethyl phenyl sulfate (4EPS) have been linked to anxiety-like behaviors and compromised brain function. These findings suggest that gut bacteria don’t just correlate with mental health—they actively influence it through their metabolic byproducts.
The inflammatory response represents another critical mechanism linking gut health to depression. When gut dysbiosis occurs, it increases intestinal permeability (often called “leaky gut”), allowing inflammatory molecules to enter systemic circulation. These inflammatory cytokines, including TNF-α, IL-6, and IL-1β, can cross the blood-brain barrier and directly affect brain function, leading to symptoms characteristic of depression and anxiety.
Clinical Evidence for Gut-Based Mental Health Interventions

The therapeutic potential of targeting gut health for mental health improvement has gained substantial scientific support. A landmark pilot study examined treatment-naïve patients with Major Depressive Disorder who received probiotic supplementation containing Lactobacillus helveticus and Bifidobacterium longum for eight weeks.
The results were remarkable: participants showed significant improvements in depression scores, with mean MADRS (Montgomery-Åsberg Depression Rating Scale) scores dropping from 24.9 at baseline to 12.7 at week eight, representing a shift from moderate to mild depression. Additionally, participants experienced reduced anxiety and improved sleep quality, with no adverse side effects reported.
These findings align with broader research showing that probiotic interventions can effectively modulate the gut-brain axis. Studies have demonstrated that specific probiotic strains can reduce the production of harmful metabolites while increasing beneficial compounds that support brain health. The anti-inflammatory effects of certain probiotics may be particularly important, as chronic inflammation is increasingly recognized as a key factor in depression development.
Practical Strategies for Supporting Gut Health and Mental Wellbeing
Dietary Interventions
Supporting gut health through nutrition involves focusing on foods that promote beneficial bacterial growth while reducing those that contribute to dysbiosis. Prebiotic-rich foods like garlic, onions, asparagus, and Jerusalem artichokes provide fuel for beneficial bacteria. Fermented foods including yogurt, kefir, sauerkraut, and kimchi introduce live beneficial bacteria directly into your system.
Reducing ultra-processed foods, excessive sugar, and artificial additives helps prevent the growth of harmful bacteria that can contribute to inflammation and mood disruption. Omega-3 fatty acids from fish, flaxseeds, and walnuts provide additional anti-inflammatory benefits that support both gut and brain health.
Probiotic Supplementation
While food sources of probiotics are valuable, targeted supplementation may be necessary for therapeutic effects. Research suggests that specific strains like Lactobacillus helveticus, Bifidobacterium longum, and Lactobacillus casei show particular promise for mood support. However, probiotic selection should ideally be guided by healthcare professionals, as different strains have varying effects.
Lifestyle Factors
Chronic stress significantly impacts gut microbiome composition through the hypothalamic-pituitary-adrenal (HPA) axis, leading to increased cortisol production and inflammatory responses. Stress management techniques like meditation, regular exercise, and adequate sleep support both gut health and mental wellbeing.
Sleep quality deserves special attention, as disrupted sleep patterns can negatively affect gut bacteria composition while gut dysbiosis can impair sleep quality, creating a vicious cycle.
Future Directions and Considerations
The field of psychobiotics—probiotics specifically targeted for mental health benefits—represents an exciting frontier in depression treatment. Researchers are exploring fecal microbiota transplantation, personalized probiotic therapies based on individual microbiome analysis, and combination approaches that integrate gut-focused interventions with traditional mental health treatments.
However, important considerations remain. The relationship between gut health and depression likely varies among individuals based on genetics, lifestyle factors, and specific microbiome compositions. More research is needed to establish optimal treatment protocols and identify which patients are most likely to benefit from gut-focused interventions.
The gut-brain connection offers hope for more holistic, personalized approaches to mental health treatment. By addressing both gut health and traditional mental health factors, we may achieve more comprehensive and sustainable improvements in depression and anxiety symptoms. As our understanding of this complex relationship continues to evolve, the integration of nutritional psychiatry with conventional treatments promises to revolutionize mental healthcare.