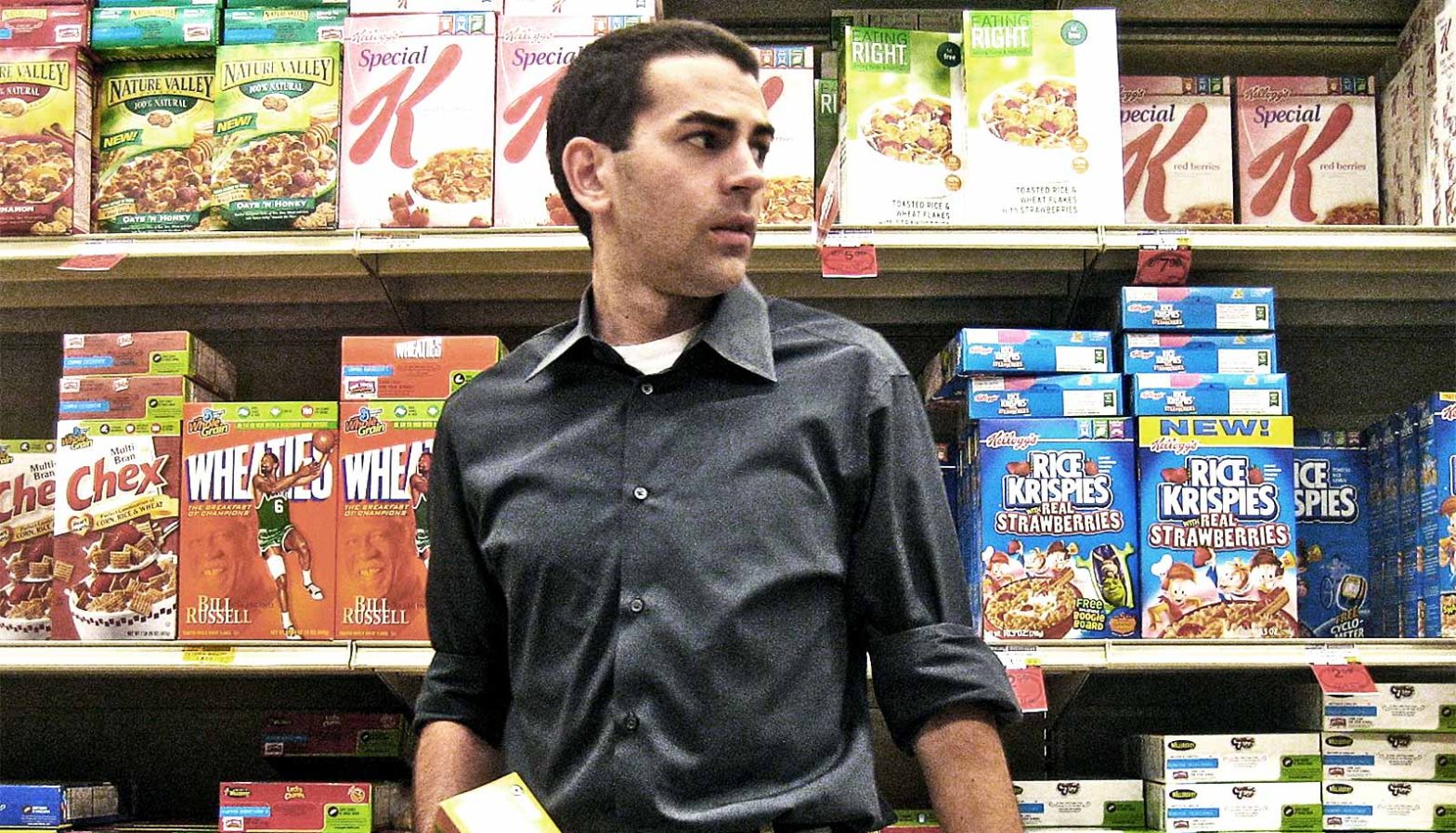
Food deserts represent one of America’s most pressing public health challenges, creating invisible barriers that separate communities from nutritious, affordable food options. These areas, predominantly found in low-income neighborhoods, lack access to full-service supermarkets and fresh produce, forcing residents to rely on convenience stores and fast-food outlets for their daily nutrition.
The consequences extend far beyond individual dietary choices, contributing to a widening gap in health outcomes between socioeconomic groups. While approximately 47 million Americans live in food deserts, recent research reveals that the relationship between food access and nutritional inequality is more complex than previously understood. Understanding this multifaceted issue is crucial for developing effective policies and interventions that can truly address the root causes of America’s nutrition divide.
Understanding Food Deserts: Definition and Geographic Distribution
Food deserts are defined by the USDA as areas where residents have limited access to fresh fruits, vegetables, and other healthful whole foods, typically due to the absence of grocery stores within a reasonable traveling distance. These areas are disproportionately concentrated in low-income and historically marginalized communities across the United States.
The geographic distribution of food deserts reveals stark disparities in food access. Urban food deserts often emerge in inner-city neighborhoods where supermarket chains have relocated to suburban areas, leaving behind smaller corner stores with limited healthy food options. Rural food deserts face different challenges, with vast distances between communities and grocery stores creating transportation barriers for residents without reliable vehicles.
Health Consequences of Limited Food Access
The health implications of living in food deserts are severe and far-reaching. Research demonstrates that residents of these areas face significantly higher risks of multiple chronic conditions:
Obesity and Weight-Related Issues: The prevalence of processed foods high in salt, sugar, and unhealthy fats contributes to elevated obesity rates in food desert communities.
Diabetes: Adults who are food insecure are two to three times more likely to develop type 2 diabetes compared to those with adequate food access.
Cardiovascular Disease: Limited access to fresh produce and whole foods increases the risk of heart disease, high blood pressure, and stroke.
Cancer: Recent studies show that Americans living in areas with poor food access are 59% more likely to die from obesity-related cancers, which account for 40% of all cancers diagnosed annually.
The life expectancy gap is particularly striking—people living in food deserts have a life expectancy of more than two years lower than those in areas with abundant healthy food access.
The Complex Reality of Nutritional Inequality

Groundbreaking research has challenged conventional assumptions about food deserts and nutritional inequality. A comprehensive study published in The Quarterly Journal of Economics found that simply improving food access addresses only a small fraction of the nutrition gap between income groups.
The research revealed that exposing low-income households to the same food products and prices available to higher-income households would reduce nutritional inequality by only 9-10%. The remaining 90% of the disparity stems from differences in food demand, suggesting that factors like education, nutritional knowledge, and cultural food preferences play larger roles than previously recognized.
This finding has significant implications for policy development, indicating that supply-side interventions alone—such as subsidizing grocery stores in underserved areas—may have limited effectiveness in addressing nutritional inequality.
Innovative Solutions and Community-Based Approaches
Despite the complexity of the issue, numerous innovative solutions are emerging to address food desert challenges:
Mobile Food Markets: These bring fresh, culturally appropriate foods directly to underserved communities, overcoming transportation barriers.
Community Food Co-ops: Worker-owned cooperatives like the Wirth Cooperative Grocery in Minneapolis provide local economic opportunities while addressing food access.
Urban Agriculture: Community gardens and vertical farming initiatives bring food production directly into neighborhoods lacking grocery stores.
Bus Stop Farmers Markets: These strategically placed markets make healthy food accessible during residents’ daily commutes.
Government Initiatives: Tax incentives for retailers, improved public transportation, and community development grants support comprehensive approaches to food access.
Moving Forward: A Holistic Approach
Addressing food deserts and nutritional inequality requires multifaceted strategies that go beyond simply increasing grocery store availability. Successful interventions must combine improved food access with nutrition education, community engagement, and policies that address underlying socioeconomic disparities.
The path forward involves collaboration between government agencies, private sector partners, and grassroots community organizations to create sustainable solutions that truly meet the needs of underserved populations.