Nick Fournie’s life took a dramatic turn when he was 24 and began experiencing severe depression. At the time, he was happily married to his long-time sweetheart, Mary, and had no reason to suspect any mental health issues. However, while mowing the lawn one day, he suddenly found himself questioning life itself, feeling as though he would be okay if it all ended. This moment marked the beginning of a long and difficult journey for Nick and Mary, as they struggled to find a solution to his worsening depression.
For nearly a decade, Nick tried various antidepressants in an attempt to alleviate his condition, but none of them worked. Mary recalled how these medications often led to intense and distressing side effects, including what Nick described as “psychotic episodes.” Despite trying ten different drugs, Nick’s depression only deepened, and he experienced bouts of paranoia and a growing inability to find joy in life. Although he managed to keep working, he felt disconnected from everything, unable to experience happiness.
In the years that followed, Nick’s condition continued to deteriorate, and he became more isolated. He struggled with severe emotional numbness, where every day felt like an eternity. After many years of failure with traditional treatments, Nick’s sister, a nurse, suggested a new approach: vagus nerve stimulation (VNS). Approved by the FDA in 2005 for chronic depression that hasn’t responded to other treatments, VNS involves stimulating the vagus nerve, a large nerve that connects the brain to various organs in the body, to improve mood regulation.
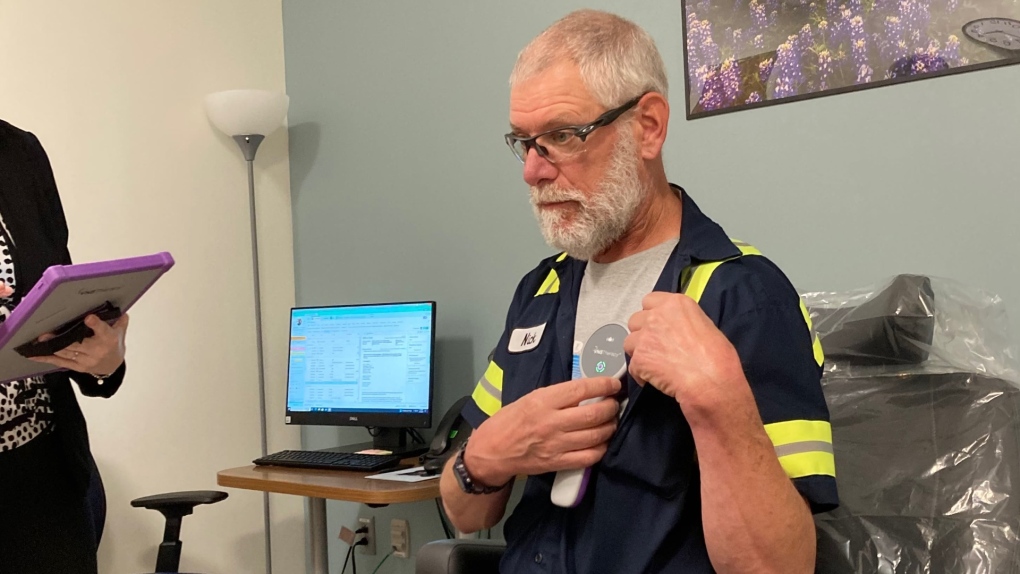
Nick decided to enroll in a clinical trial for VNS led by Dr. Charles Conway, a professor of psychiatry. A small device, similar to a pacemaker, was implanted under his collarbone, and a lead was placed near the neck to stimulate the vagus nerve. The device delivered regular pulses to the brain, which began to bring significant improvements to Nick’s condition over time. For the first time in years, Nick experienced joy and a renewed sense of purpose.
In addition to the VNS treatment, Nick continued to work with his doctor to manage his antidepressants, alternating between two medications to find the most effective combination. Mary expressed how this combination of VNS and medication truly transformed Nick’s life, restoring not only his mental health but also the joy in their relationship. She credited VNS with saving both Nick’s life and their marriage, though she acknowledged that it was not a “magic bullet” and still required behavioral changes and coping strategies.
Despite the positive effects of VNS, insurance coverage was a significant hurdle. When the therapy was first FDA-approved, the Centers for Medicare and Medicaid Services (CMS) rejected its coverage in 2007, citing insufficient evidence. However, as more research supported its benefits, CMS reversed its decision in 2019, allowing coverage under certain conditions, though many private insurers still did not cover the treatment, making it financially inaccessible for many.
A major clinical trial began in 2019 to study the effectiveness of VNS for treatment-resistant depression, involving 493 adults who had all failed at least 13 prior treatments. The results, published in 2024, confirmed the effectiveness of VNS for improving depressive symptoms, daily functioning, and overall quality of life. While the primary goal of the trial was not met, the secondary outcomes showed significant improvements, with 18% of participants experiencing a dramatic reduction in symptoms and over half reporting a better quality of life.
The trial also highlighted the challenges of treating the most severe cases of depression, with some participants having struggled with the illness for decades. Despite these challenges, researchers found that VNS therapy led to noticeable improvements for many patients. The study’s findings were particularly encouraging for those who had not responded to other treatments, suggesting that VNS might be an important option for people with chronic, treatment-resistant depression.
Although VNS can cause side effects, such as shortness of breath or hoarseness, it remains a promising treatment for severe depression. The mechanisms through which VNS works are still being studied, but experts believe that the therapy helps regulate brain networks involved in mood regulation, increases levels of mood-regulating chemicals like serotonin and norepinephrine, and may also reduce inflammation, a factor linked to depression.
The ongoing research into VNS therapy provides hope for many patients who suffer from treatment-resistant depression. However, its high cost and limited insurance coverage remain significant obstacles. As more studies demonstrate its effectiveness, there is hope that VNS will become a more widely available treatment option. For now, patients seeking VNS therapy may need to explore private insurance options or consider participation in clinical trials to access this potentially life-changing treatment.
The clinical trial results, along with Nick Fournie’s personal success with VNS, underscore the importance of finding new approaches to treating depression, especially for those who have not found relief through traditional methods. The story of Nick and Mary Fournie is a testament to the resilience of individuals battling severe mental illness and the potential for innovative therapies like VNS to bring lasting improvements to their lives.
