The sole HIV vaccine in an advanced-stage trial has failed, researchers announced on Wednesday, delivering a significant setback to efforts to combat the global HIV epidemic and adding to decades of unsuccessful attempts.
Known as Mosaico, the trial was a collaboration between the U.S. government, pharmaceutical giant Janssen, and other partners.
It spanned eight countries across Europe and the Americas, including the U.S., and began in 2019. The study enrolled nearly 3,900 men who have sex with men and transgender individuals, all assessed to be at high risk of contracting HIV.
Following a review of the trial’s findings by an independent data and safety monitoring board, the study leaders decided to halt the extensive research effort when no evidence was found that the vaccine reduced the rate of HIV acquisition among participants.
“It’s obviously disappointing,” remarked Dr. Anthony Fauci, long-time director of the National Institute of Allergy and Infectious Diseases and a pivotal figure in the trial. However, he remains optimistic about other promising approaches in early stages of HIV vaccine research.
Fauci, who retired recently without achieving his goal of proving an HIV vaccine at least 50% effective, emphasized that the field of HIV vaccine development should not be abandoned despite this setback.
The trial, supported by the HIV Vaccine Trials Network, the Fred Hutchinson Research Center, and the U.S. Army Medical Research and Development Command, saw its efficacy findings in line with expectations following the previous failure of a similar vaccine trial called Imbokodo, which targeted women in Africa and was announced in August 2021.
The combined cost for both trials amounted to $56 million according to an NIAID spokesperson.
Both Mosaico and Imbokodo utilized vaccines employing a common cold virus to deliver mosaic immunogens, designed to provoke a robust immune response by including genetic material from various prevalent HIV strains globally. Mosaico incorporated an additional element to broaden the immune reaction.
Participants aged 18 to 60 received either the vaccine or a placebo through four injections over 12 months. The monitoring board found no significant difference in HIV acquisition rates between the two groups.
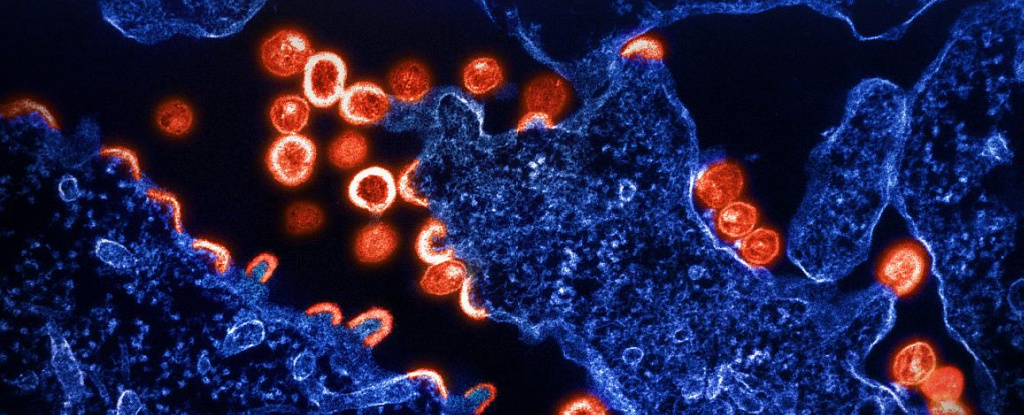
Fauci highlighted a critical limitation of the Mosaico vaccine: its elicitation of non-neutralizing antibodies against HIV instead of neutralizing antibodies, which are essential for effectiveness.
Looking ahead, Fauci sees promise in upcoming HIV vaccine innovations, particularly those leveraging mRNA vaccine technology akin to some COVID-19 vaccines.
The enduring challenge in HIV vaccine research, Fauci stressed, lies in surpassing the natural immune response to infection, which has proven inadequate against the virus.
The Mosaico trial’s failure underscores the formidable hurdles in developing an effective HIV vaccine, despite numerous global efforts since the virus was identified in 1984.
Of the nine late-stage clinical trials conducted thus far, including Mosaico and Imbokodo, only one demonstrated any efficacy — albeit at a modest level insufficient for regulatory approval. This trial, conducted in Thailand between 2003 and 2006, published its findings in 2009.
Despite setbacks, insights from the Thai trial continue to inform ongoing HIV vaccine research globally, including the design of subsequent trials like Imbokodo and Mosaico.
Dr. Susan Buchbinder, co-leader of the Mosaico trial and an epidemiologist at the University of California, San Francisco, expressed optimism about analyzing participant blood samples in the coming months to uncover potential reasons for the vaccine’s failure and identify subgroups where efficacy might be detected.
Reflecting on the trial’s outcome, Jennifer Kates, Director of Global Health and HIV Policy at Kaiser Family Foundation, emphasized the continued importance of HIV vaccine research despite its challenges.
While the development of an effective HIV vaccine remains elusive, Kates highlighted existing highly effective HIV prevention strategies, such as pre-exposure prophylaxis (PrEP), voluntary medical male circumcision, and antiretroviral treatment, which have made significant strides in reducing HIV transmission globally.
Globally, approximately 38.4 million people were living with HIV in 2021, and efforts to control the virus have seen annual infection rates halved since 1996.
Fauci concluded by underscoring the ethical complexities of designing trials like Mosaico in the era of PrEP availability, which necessitates enrolling participants still at substantial risk of HIV.
