The Biden administration has decided to extend the Covid-19 public health emergency until April, citing concerns over a highly transmissible omicron subvariant that could potentially lead to another wave of hospitalizations in the U.S. this winter.
“The COVID-19 Public Health Emergency remains in effect, and as HHS committed to earlier, we will provide a 60-day notice to states before any possible termination or expiration,” stated a spokesperson from the Health and Human Services Department.
Since its initial declaration by the Trump administration in January 2020, the U.S. has regularly renewed the Covid public health emergency every 90 days.
The emergency status has significantly impacted the U.S. healthcare system over the past three years, ensuring continuity of public health insurance coverage for millions, granting hospitals flexibility to manage patient surges, and facilitating the expansion of telehealth services.
The White House Covid task force, led by Dr. Ashish Jha, has emphasized that the U.S. is now better equipped due to widespread vaccination availability and effective treatments that mitigate severe illness and death from the virus.
In August, the Department of Health and Human Services (HHS) advised state and local health authorities to prepare for the eventual end of the emergency.
HHS has committed to providing a 60-day notice period to state governments and healthcare providers before lifting the emergency declaration.
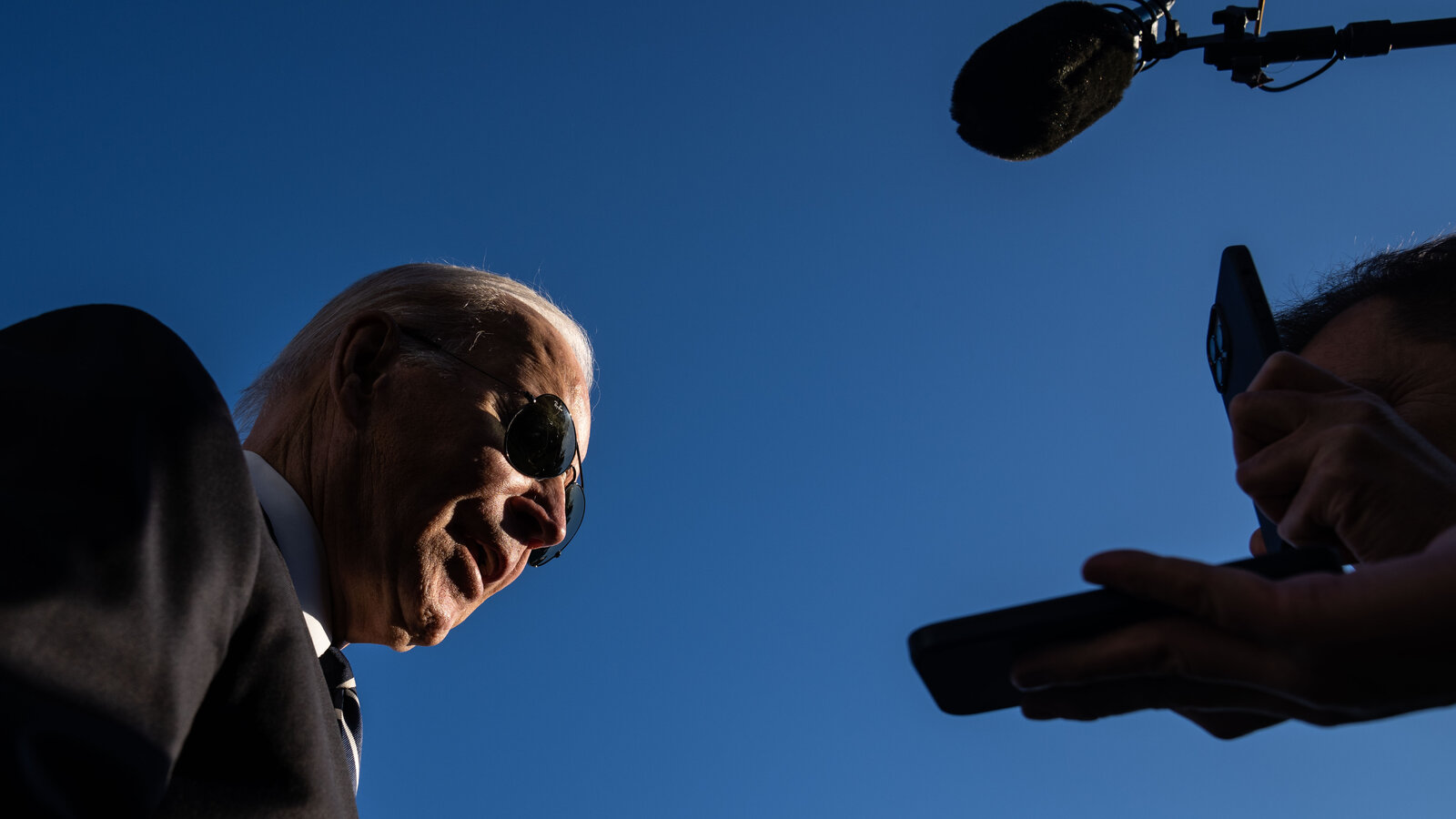
President Joe Biden previously declared the pandemic over in September amid declining infection rates, hospitalizations, and deaths.
However, HHS Secretary Xavier Becerra cautioned in October that the trajectory of the virus during the winter months would determine whether continuation of the emergency was necessary.
When the decision is made to end the public health emergency, hospitals will lose the flexibility to adjust staffing levels, expand bed capacity, and manage patient care during surges in admissions.
Additionally, the expanded role of pharmacies in vaccine administration during the pandemic may be affected, although the extent of this impact remains unclear.

Millions of Americans are anticipated to lose Medicaid coverage in the coming months, as Congress had prohibited states from disenrolling individuals from the program for the duration of the public health emergency.
Last month, Congress separated these Medicaid protections from the emergency declaration, allowing states to begin terminating Medicaid coverage for ineligible individuals starting in April.
The omicron XBB.1.5 subvariant, which is rapidly spreading in the U.S., has raised concerns among scientists due to its enhanced ability to bind to human cells and evade immunity.
The World Health Organization has identified it as the most transmissible omicron subvariant thus far, although current data does not suggest it causes more severe illness.
Since the arrival of omicron in late 2021, the virus has evolved into various subvariants that are increasingly adept at evading immunity conferred by vaccination or prior infection.
A recent study by Columbia University highlighted the BQ and XBB families of omicron subvariants as posing significant challenges to Covid vaccines, potentially leading to an increase in breakthrough infections.
These subvariants have also shown resistance to authorized antibody treatments used to protect immunocompromised individuals.
Dr. Ashish Jha expressed concern on Twitter about the rapid spread of XBB.1.5 but noted that it does not represent a major setback.
He urged eligible individuals to receive an omicron booster shot and advised vulnerable populations to seek antiviral treatment if infected with the virus.
Data from the Centers for Disease Control and Prevention indicates that only 38% of seniors aged 65 and older have received an omicron booster, raising concerns about potential increases in hospitalizations and deaths among this age group as XBB.1.5 continues to circulate.
Jha emphasized that most Covid-related hospitalizations and deaths currently involve individuals aged 70 and older who are either unvaccinated or inadequately treated following breakthrough infections.