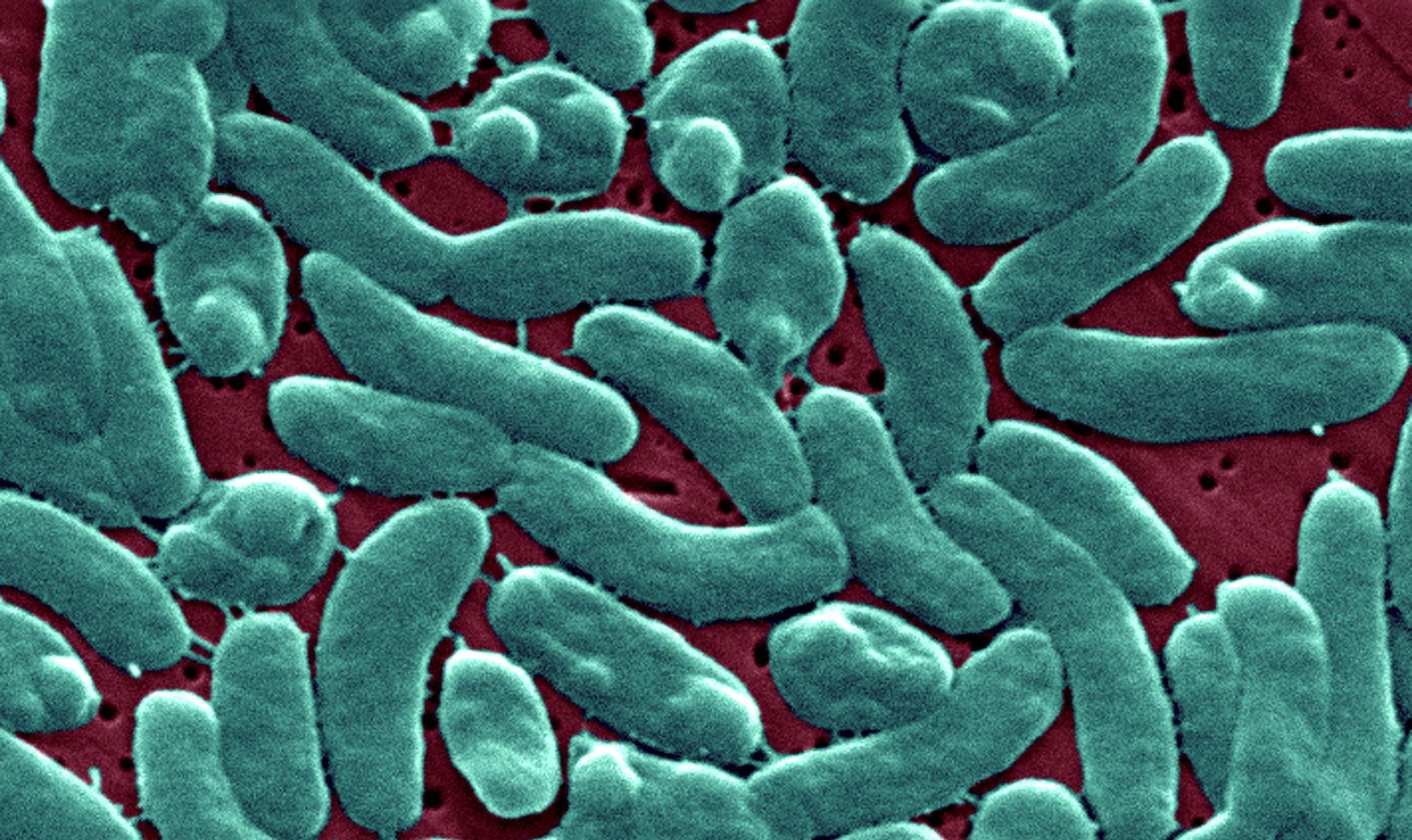
The US Centers for Disease Control and Prevention (CDC) issued a national health alert on Friday, urging clinicians to be vigilant for infections caused by the flesh-eating bacteria Vibrio vulnificus.
During July and August, as the US experienced widespread heatwaves and higher-than-average coastal sea surface temperatures, severe and fatal V. vulnificus infections were reported in Connecticut, New York, and North Carolina. At least five people have died in these states.
The bacteria naturally inhabit coastal waters and thrive in the warmer months when ocean temperatures are at their peak.
“Three people have died after infection with rare flesh-eating bacteria in Connecticut and New York,” reported the CDC.
While most infections occur after consuming raw or undercooked seafood, individuals can also become infected by swimming in the ocean with an open wound, such as a recent piercing, tattoo, or even a minor cut or scrape.
Exposure to the bacteria can also happen when hurricanes, floods, and storm surges push coastal waters inland.
For instance, in the aftermath of Hurricane Ian last year, Florida health officials reported 38 cases and 11 vibriosis-related deaths linked to the storm.
Historically, the bulk of US infections were reported by residents of Gulf Coast states, as the bacteria prefer warmer temperatures. However, as the climate crisis heats the oceans and brings more heatwaves, an increasing number of cases have been treated in states along the East Coast.
The CDC estimates that the US typically sees about 80,000 illnesses connected to Vibrio bacteria each year. While not all species are “flesh-eating,” about a dozen species can make humans sick, causing symptoms such as diarrhea, stomach cramps, nausea, vomiting, fever, and chills.
“Georgia resident dies from rare brain-eating amoeba, health officials say,” the CDC noted.
Vibrio vulnificus is among the bacteria that can cause what is commonly known as a flesh-eating infection.
Of the 150 to 200 cases of Vibrio vulnificus reported to the CDC annually, about 1 in 5 die from the infection, sometimes within one or two days of falling ill.
Necrotizing fasciitis, which the bacteria can cause, eats away at the skin, muscles, nerves, fat, and blood vessels around an infected wound.
In more severe cases, septicemia can develop, particularly in individuals with underlying health conditions like liver disease, cancer, diabetes, HIV, or other immune-suppressing diseases.
Septicemia occurs when the bacteria enter the bloodstream and spread, causing fever, chills, low blood pressure, or skin blisters. This can lead to septic shock, where blood pressure drops dangerously.
The bacteria release toxins into the bloodstream that can cause extremely slow blood flow, damaging tissue and organs.
Sepsis, another potential consequence, is when the body mounts a strong immune response that shuts down vital organs like the heart or kidneys.
Acute respiratory distress syndrome (ARDS) can also occur, where oxygen from the lungs doesn’t reach the blood, potentially causing brain damage and permanent lung damage.
If the infection spreads into the bloodstream, it can be fatal.
The fatality rate is about 25% for wound infections, and studies show it’s much higher for those exposed to the bacteria by consuming contaminated food.
For skin infections, doctors take samples from the infected area to identify Vibrio vulnificus as the cause. Treatment includes draining any abscesses and addressing the infected site.
In cases of necrotizing fasciitis, surgery or even amputation may be necessary to prevent the infection from spreading.
The CDC advises prompt treatment for suspected infections to improve survival chances. Some strains of this bacteria have developed antimicrobial resistance, and about 50% of infections no longer respond to antibiotics.
To avoid Vibrio infection, the CDC recommends ensuring seafood is well-cooked, avoiding raw or undercooked oysters and other shellfish, and washing hands after handling raw seafood.
People with skin wounds should avoid the ocean and brackish water or cover the wound with waterproof bandages.
After exposure to salt or brackish water, thorough washing of hands and any cuts with soap and water is highly recommended. For those cleaning up after flooding or hurricanes, wearing protective shoes and clothing is advised.