European drug authorities have issued recommendations aimed at addressing the persistent shortages of glucagon-like peptide 1 (GLP-1) receptor agonists, which are utilized in the treatment of type 2 diabetes and obesity.
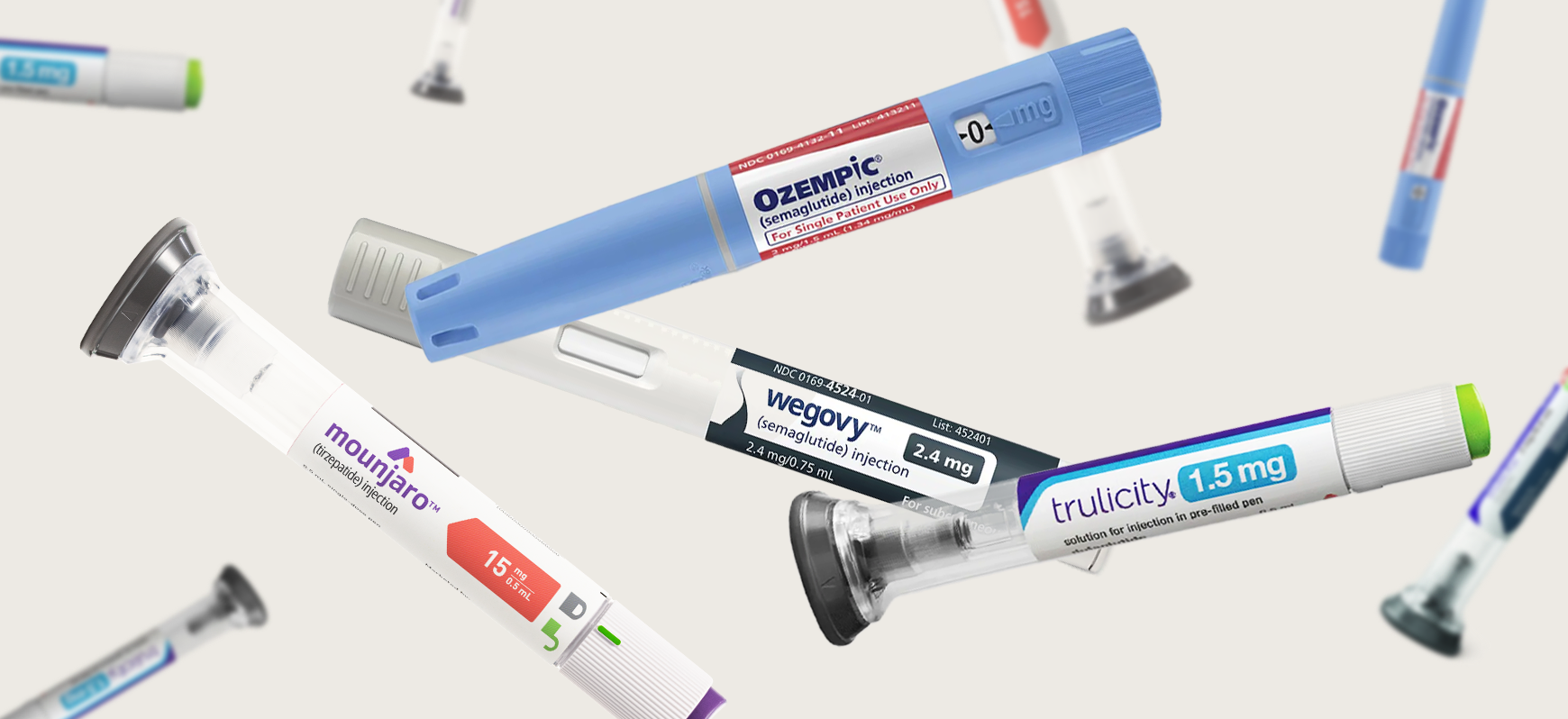
These medications include Ozempic (semaglutide), Saxenda (liraglutide), Trulicity (dulaglutide), and Victoza (liraglutide).
Since 2022, GLP-1 receptor agonists have gained popularity on social media, with influential figures endorsing them as miraculous weight loss solutions.
However, their off-label use, particularly among individuals who do not have diabetes or obesity, is worsening drug shortages and posing risks to public health.
In response, the European Medicines Agency (EMA) and the Heads of Medicines Agencies (HMA) have reiterated to healthcare professionals that these medications should only be prescribed for their approved indications, emphasizing the necessity of adhering to national guidelines.
Karl Broich, chair of the HMA and president of the Federal Institute for Drugs and Medical Devices, underscored the significance of these recommendations, stating,
“The recommendations are a reminder that any use outside of the indications of the individual medicines is considered off-label and that this use will aggravate existing shortages.”
He highlighted that healthcare professionals should not prescribe these medications for cosmetic weight loss in individuals without obesity or related health issues and should instead promote lifestyle changes for those seeking to lose weight without underlying conditions.
Broich pointed out that off-label use can compromise patient safety due to the potential severe side effects associated with GLP-1 agonists.
He urged that these medications be prioritized for patients with legitimate medical needs to ensure their availability during shortages.
Emer Cooke, executive director of the EMA, emphasized the broader public health implications, noting that one in six Europeans currently experiences obesity and that the number of individuals with diabetes in the EU is projected to reach 38 million by 2030.

“The demand for these medicines continues to increase, and the current supply cannot keep up,” she stated, highlighting the risks posed by shortages to those in genuine need of these treatments.
Euan Woodward, executive director of the European Association for the Study of Obesity, expressed concern regarding the potential for medication discontinuation among patients prescribed GLP-1 agonists.
This could lead to increased stress and cortisol levels, possibly resulting in weight regain and a decreased quality of life.
The heightened demand for GLP-1 agonists has also given rise to an online market for substandard and counterfeit medications. 3
Cooke warned that the use of falsified products can have serious health consequences, advising patients to obtain GLP-1 receptor agonists solely through medical prescriptions or from pharmacies that are accredited by national authorities within EU Member States.
“There are some rogue actors claiming to supply weight loss medicines, and it’s very important that consumers realize the potential risks of these unauthorized products,” she remarked.
“Shortages are a major public health concern, and they require urgent and coordinated action across member states and various stakeholders, including industry, regulators, prescribers, healthcare professionals, pharmacists, and patients,” Cooke emphasized.
The EMA and HMA recommendations are part of a wider initiative by the EMA to tackle GLP-1 agonist shortages. The agency is actively collaborating with pharmaceutical companies to monitor the situation and provide guidance on increasing manufacturing capacity.
However, scaling up production involves complex processes such as setting up new manufacturing sites or adding filling lines, which are especially challenging for these intricate medications.
Moreover, the EMA is facilitating stock redistribution among member states, sharing best practices, and regulating the number of prescriptions that pharmacies can dispense, alongside prescription limits and reimbursement controls.
“Despite these efforts, we are concerned that our messages don’t always reach the healthcare providers and patients whose actions can significantly impact managing these shortages,” Cooke acknowledged.
Broich encouraged companies to reconsider their promotional activities during the shortage. “As long as the shortage persists, we should avoid promotional activities.
Claims made should align with the rational use of these medicines and public health goals. Companies should also run awareness campaigns about weight management and educational initiatives concerning the ongoing shortage and its clinical implications.”
The MSSG has committed to conducting a study utilizing real-world data (via DARWIN EU) to better understand the actual usage of these medicines. Preliminary results are expected by the end of August, providing insights into practical use, according to Cooke.