Earlier this month, a mysterious flu-like illness in the Democratic Republic of Congo (DRC) alarmed health officials, with dozens of deaths reported over several months. The World Health Organization (WHO) and local authorities launched an investigation, and by December 17, they identified severe malaria, potentially complicated by malnutrition, as the likely cause. However, the situation became more complex when, two days later, a man in the affected region died with symptoms of hemorrhagic fever, raising concerns that malaria and malnutrition alone might not fully explain the outbreak. The reported case count had reached 592, with confirmed and suspected deaths ranging from 67 to 143.
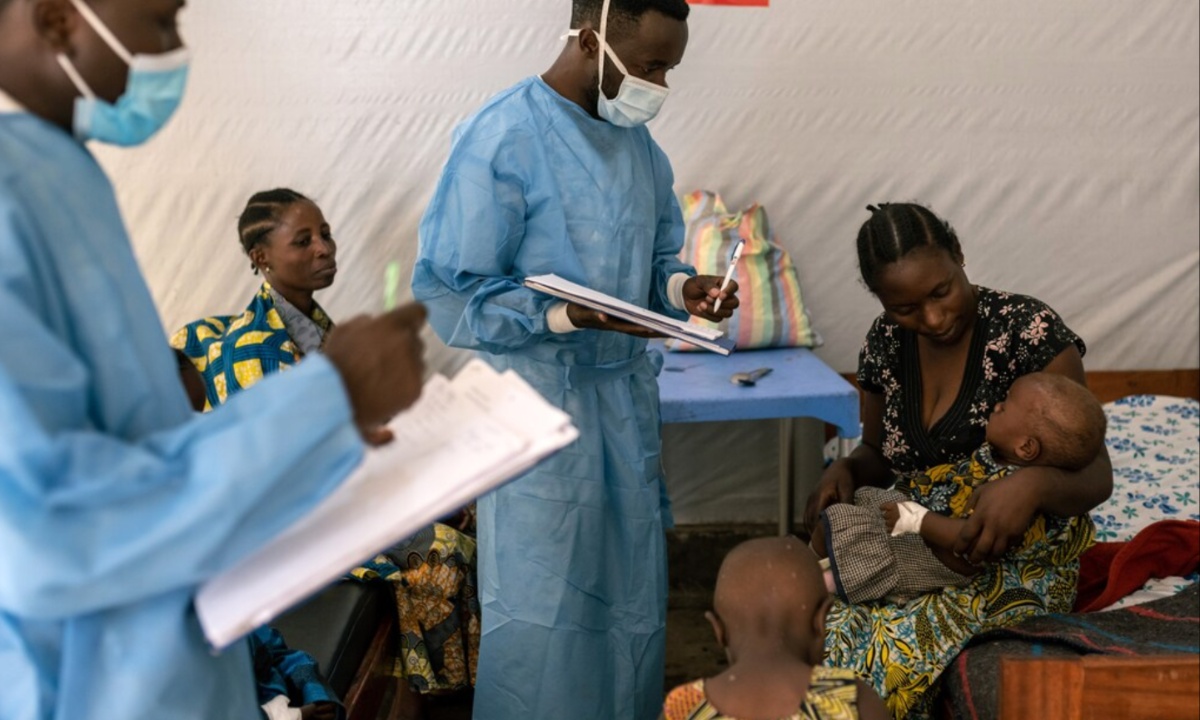
Diagnosing the illnesses has been particularly challenging due to the high prevalence of malaria in the DRC. Many individuals in malaria-endemic regions carry parasites in their blood without showing symptoms, making it difficult to determine if malaria is the primary cause of the outbreak. Experts like Dr. Benjamin Mordmüller emphasize the need for diagnostic tests to differentiate malaria from other diseases with similar symptoms, such as fever and fatigue. Unfortunately, the lack of local laboratory facilities means that samples must be sent to Kinshasa for analysis, significantly delaying results.

Geographic and seasonal factors have further complicated the response. The outbreak is concentrated in the remote Panzi health zone of the Kwango province, which takes 48 hours to reach by road from Kinshasa. The rainy season has made transportation more difficult and increased mosquito breeding, potentially driving up malaria cases. Some symptoms observed in patients, such as runny noses and coughs, are not typical of malaria and may indicate co-infections. Severe cases involving respiratory distress and acute malnutrition suggest a complex interplay between malnutrition and malaria that remains poorly understood.
Food insecurity, worsened by climate-related droughts earlier in 2024, has exacerbated the crisis in Kwango province. Malnutrition may influence the severity of malaria, but its effects are not uniform; in some cases, it might amplify malaria’s impact, while in others, it could suppress symptoms. Efforts to address the outbreak include the distribution of malaria medications and diagnostic tools, but limited infrastructure and communication networks in the region continue to hinder progress.
The situation remains fluid, as health officials explore the possibility of additional diseases contributing to the outbreak. The appearance of hemorrhagic fever suggests that a viral infection might also be at play. WHO officials and experts agree that the outbreak may involve multiple factors, with severe malaria and malnutrition playing key roles but not providing the full explanation. Further investigation and improved access to healthcare resources are critical to fully understanding and addressing this complex health emergency.