The United States has witnessed a significant decline in triplet and higher-order multiple births over the past few decades, with rates dropping by 62% from 1998 to 2023. A report from the Centers for Disease Control and Prevention (CDC) highlights that this decline is particularly pronounced among mothers aged 30 and older. The decrease is largely attributed to strengthened medical guidelines regarding assisted reproductive technologies (ART), including in vitro fertilization (IVF), which recommend limiting the number of embryos transferred during fertility treatments.
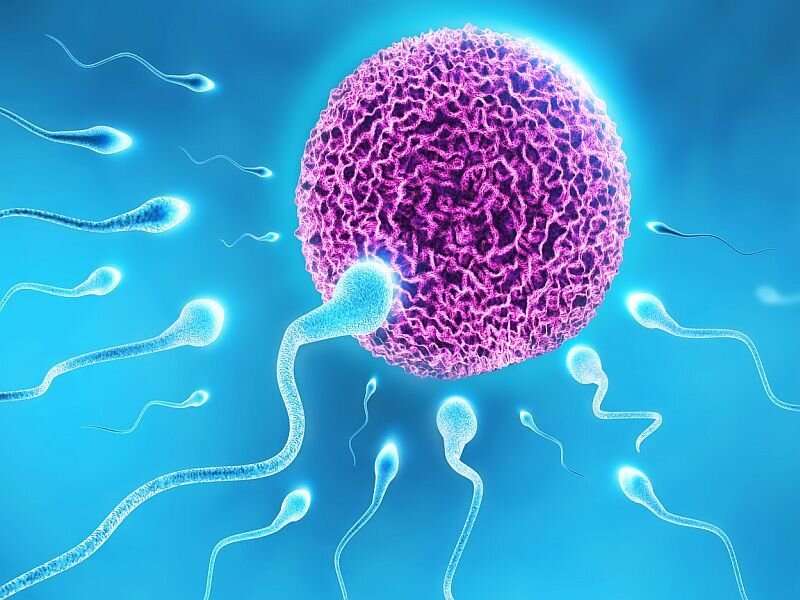
Historically, the use of ART, especially IVF, has been associated with an increase in multiple births, as transferring multiple embryos enhances the likelihood of conception. However, Joyce Martin, a researcher at the CDC, points out that pregnancies involving triplets or more come with increased risks for mothers and infants, such as complications during pregnancy, preterm birth, and higher infant mortality rates. This recognition has prompted a reevaluation of practices surrounding embryo transfers in fertility treatments.
The rise of multiple births in the late 20th century correlates with the mainstream adoption of fertility treatments following the 1980s. In response to concerns about the health risks of multiple pregnancies, professional organizations like the American Society for Reproductive Medicine initiated guidelines in the early 2000s aimed at reducing the number of embryos transferred. Over the years, these guidelines have evolved, becoming stricter in light of advancements in reproductive technology and the increasing need to ensure safer fertility treatment outcomes.
The most recent guidelines, published in 2021, recommend that women under 35 should typically undergo single embryo transfers, while women over 40 are advised to limit transfers to no more than four untested early-stage embryos. Alongside these recommendations, there has also been a rise in the practice of fetal reduction, which involves reducing the number of fetuses in cases of triplet pregnancies or more. Maternal health experts view this shift as beneficial, as it can substantially lower the risks associated with carrying multiple fetuses.
The statistical data reveals a dramatic increase in triplet and higher-order births from 37 per 100,000 births in 1980 to a peak of around 194 per 100,000 in 1998. Since then, the rate has declined to approximately 74 per 100,000 births, marking a notable reduction in both the incidence and the absolute number of such births. The sharpest decline has been observed since 2009 when high-profile cases such as Nadya Suleman’s octuplets brought significant attention to the public health concerns surrounding multiple pregnancies.
Analyzing the data by maternal age shows that all age groups have experienced declines in triplet and higher-order multiple birth rates, with the most significant reductions occurring among women in their 30s and 40s. Racial disparities are also evident in these trends. For instance, the rate of triplet and higher-order births among White mothers fell by 71%, while Hispanic mothers experienced a 25% decrease. Conversely, Black mothers saw an overall increase of 25%, suggesting differences in access to advanced reproductive technologies.
Experts highlight that these racial disparities may stem from varying levels of access to effective fertility treatments. Many Black women and low-income mothers often resort to less advanced methods of assisted reproductive technology, leading to higher chances of multiple births.
This disparity underscores the importance of ensuring equitable access to reproductive healthcare. While the overall trend indicates success in reducing triplet and higher-order births through the implementation of ART guidelines, it also calls for continued efforts to address disparities in access and outcomes across different demographic groups.
