The class of weight loss medications known as GLP-1 inhibitors, including Ozempic and Wegovy, are increasingly recognized for their broad health benefits. Initially hailed for their effectiveness in treating obesity and diabetes, these drugs are now being associated with reduced risks of other conditions like heart disease and chronic kidney disease.
Recent research from Brigham and Women’s Hospital adds to their growing list of benefits, revealing that during the COVID-19 pandemic, GLP-1 inhibitors reduced the risk of COVID-19-related deaths among obese and overweight patients by nearly 20%. This finding could have significant implications for treating conditions commonly linked with metabolic diseases.
The study, led by Dr. Benjamin M. Scirica, focused on reanalyzing data from a trial originally designed to evaluate the cardiovascular effects of semaglutide, the active ingredient in Ozempic and Wegovy.
While the trial initially aimed to assess the drug’s impact on cardiovascular events in patients with metabolic syndrome, it unexpectedly revealed a reduction in non-cardiovascular deaths, particularly during the COVID-19 pandemic. This discovery was presented at the European Society of Cardiology Congress 2024 and has sparked new interest in the potential broader applications of GLP-1 inhibitors.
Originally, the trial enrolled patients who were either pre-diabetic or obese to test whether semaglutide could prevent cardiovascular events. However, the onset of the COVID-19 pandemic led researchers to expand their data collection to include COVID-related complications and deaths.
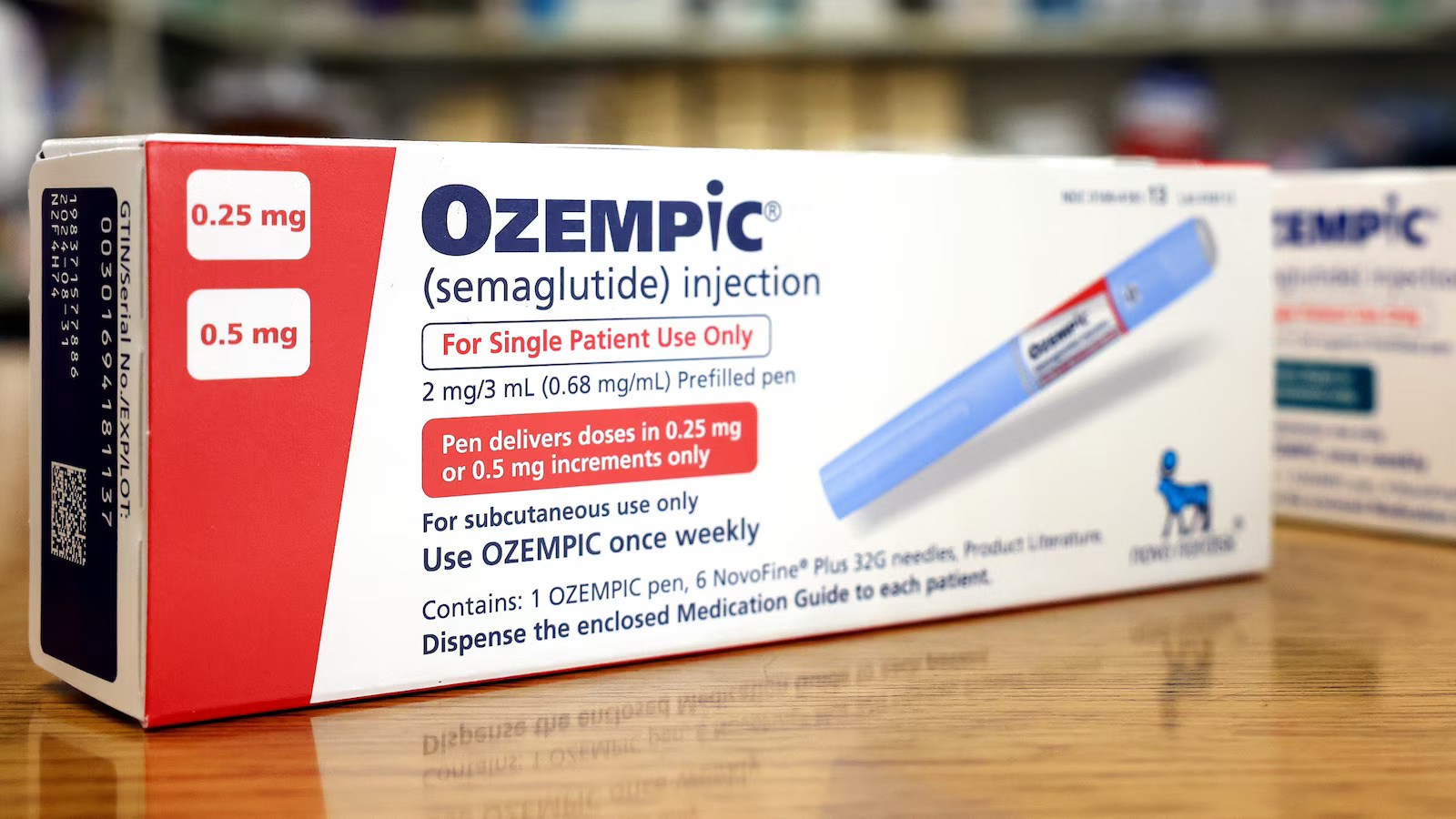
Despite initial expectations that the drug would primarily reduce cardiovascular deaths, the reanalysis showed that patients receiving semaglutide were significantly less likely to die from COVID-19 complications, suggesting the drug may have protective effects beyond its intended use.
The study’s results have been met with enthusiasm from the medical community. Dr. Jeremy Faust, a public health expert, highlighted the significance of these findings, noting that the rapid impact of semaglutide on reducing COVID-19 mortality is particularly remarkable.
The exact mechanisms by which semaglutide achieves these effects are still unclear, but researchers speculate that its benefits may stem from overall health improvements in patients, including better kidney and liver function, and potentially reduced inflammation, which is crucial in severe COVID-19 cases.
GLP-1 drugs function by activating receptors that influence insulin secretion and appetite, though their full range of effects is not yet completely understood. The popularity of these drugs has surged, especially with the introduction of semaglutide, leading to widespread use among those seeking to manage obesity and related conditions.
However, access to these medications remains uneven, with disparities in insurance coverage preventing many from benefiting from them, particularly among disadvantaged populations.
The growing recognition of GLP-1 inhibitors’ benefits has also underscored significant inequities in healthcare access. While some insurance plans cover these drugs for heart disease, Medicare does not cover them for weight loss, and Medicaid coverage varies by state.
As a result, many individuals, particularly those from marginalized communities who are disproportionately affected by conditions like obesity and diabetes, may struggle to afford these potentially life-saving treatments, exacerbating existing health disparities.
