Depression and memory decline are closely intertwined, with recent research indicating that each condition might influence the other.
According to the U.S. Centers for Disease Control and Prevention, nearly 20% of American adults aged 65 and older experience depressive symptoms.
Meanwhile, around 66% of Americans aged 70 and over face some level of cognitive impairment.
Dorina Cadar, a research fellow in dementia at University College London and a professor at Brighton and Sussex Medical School in the U.K., noted, “It is known that depression and poor memory often occur together in older people, but what comes first has been unclear.”
To investigate these connections, Cadar and her team analyzed data from 8,268 adults in England, with an average age of 64.
Over a span of 16 years, participants answered various questions regarding their mental and cognitive health.
The study found that those with higher depressive symptoms were more likely to experience faster memory decline.
Conversely, individuals who began with poorer memory were more prone to developing depressive symptoms during the study period.
Cadar told Newsweek, “The study highlights the bidirectional relationship between depressive symptoms and memory decline in older adults.
This interrelationship suggests that monitoring and addressing both aspects simultaneously might be critical for improving cognitive and emotional health.”
She also remarked, “The findings underscore the importance of early detection and intervention for depressive symptoms to potentially mitigate subsequent memory decline.
Moreover, addressing memory issues early might prevent or reduce the severity of depressive symptoms, creating a more holistic approach to managing the health of older adults.”
As the study was based on observational data, further research is necessary to confirm the neurological mechanisms underlying this association.
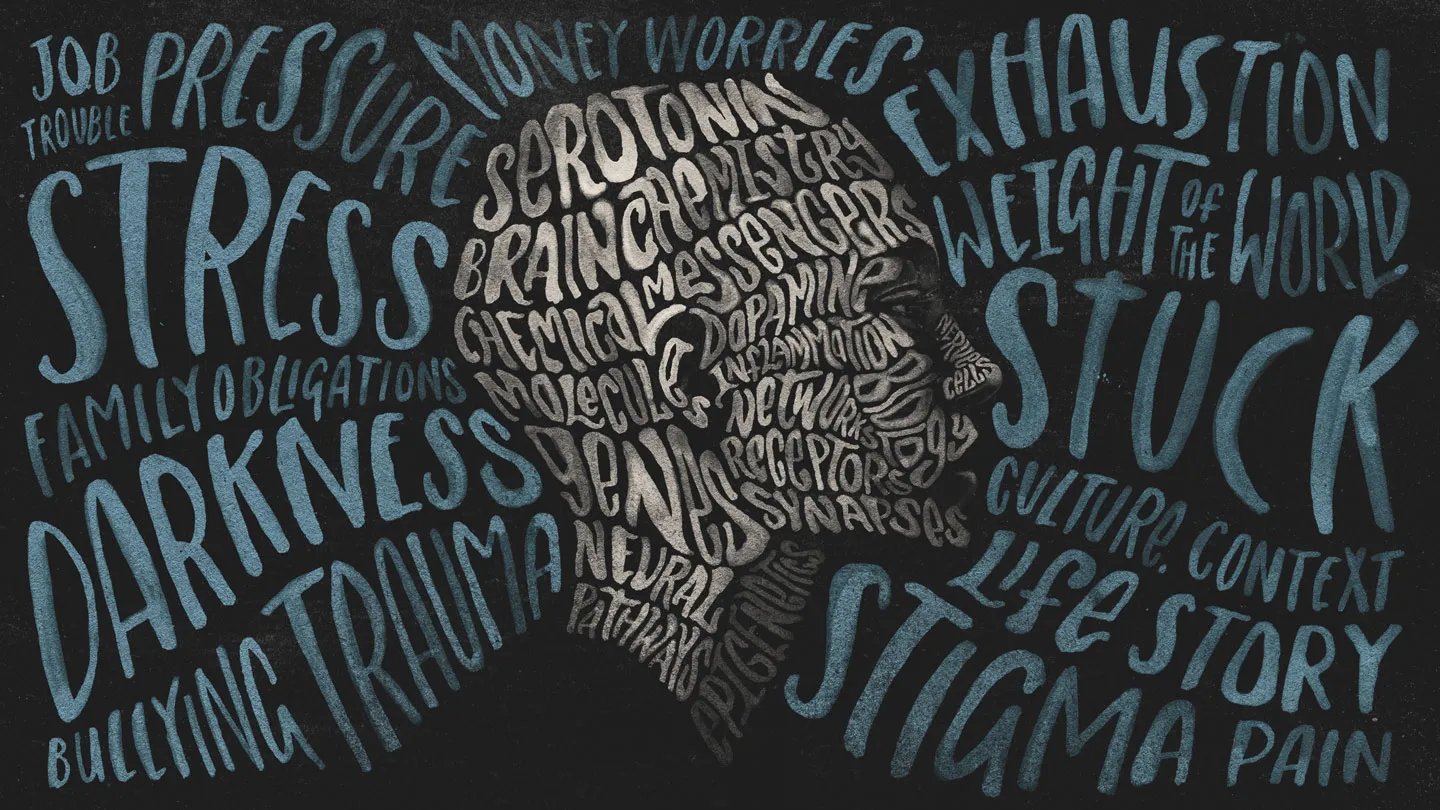
Cadar explained that changes in the brain during depressive episodes may play a role.
“Depression can cause changes in brain structures, such as the hippocampus, which is critical for memory formation and retrieval. Chronic stress and high levels of cortisol associated with depression can damage neurons in these areas.”
She added, “A further understanding of mechanisms linking memory decline and depression is crucial for developing targeted interventions aimed at improving mood and slowing cognitive decline in individuals with depression and memory impairment.”
The researchers also suggested that depressive symptoms might arise from frustration, loss of confidence, and feelings of incompetence related to age-associated memory lapses.
Cadar emphasized, “Further research into the mechanisms linking depression and memory decline, including neurochemical and structural brain changes, could provide deeper insights into effective interventions.”
Regarding whether antidepressants could help prevent memory decline, Cadar stated, “The study suggests that interventions to reduce depressive symptoms may help to slow down memory decline, but it does not specifically mention antidepressants or other forms of treatment.”
She noted, “Antidepressants are one form of intervention, and if they effectively reduce depressive symptoms, they might indirectly slow memory decline. Other forms of intervention are counseling and cognitive behavioral therapy (CBT).
However, the relationship between depression, memory decline, and the use of antidepressants or other therapies would require targeted research to confirm whether antidepressants specifically could help in slowing memory decline.”
