The anticipated joy of a new mother, who had given birth at 42 after a long-awaited pregnancy, quickly turned into a struggle when she developed postpartum depression within a week of delivery.
Postpartum depression—characterized by extreme sadness, anxiety, or despair following childbirth—affects up to 1 in 5 women.
At five months postpartum, the woman was trapped in a fog, according to Dr. Misty Richards, medical director of perinatal psychiatry at the Maternal Outpatient Mental Health Services Clinic at UCLA Health, who treated the patient and shared her experience.
“She wasn’t taking showers. She wasn’t eating,” Richards said, noting that the woman’s husband had taken a leave of absence from work to care for his wife and their newborn.
Richards’ clinic has dealt with numerous cases like this. Initially, she referred the woman to an intensive outpatient program, but even while participating, the patient remained actively suicidal, Richards reported.
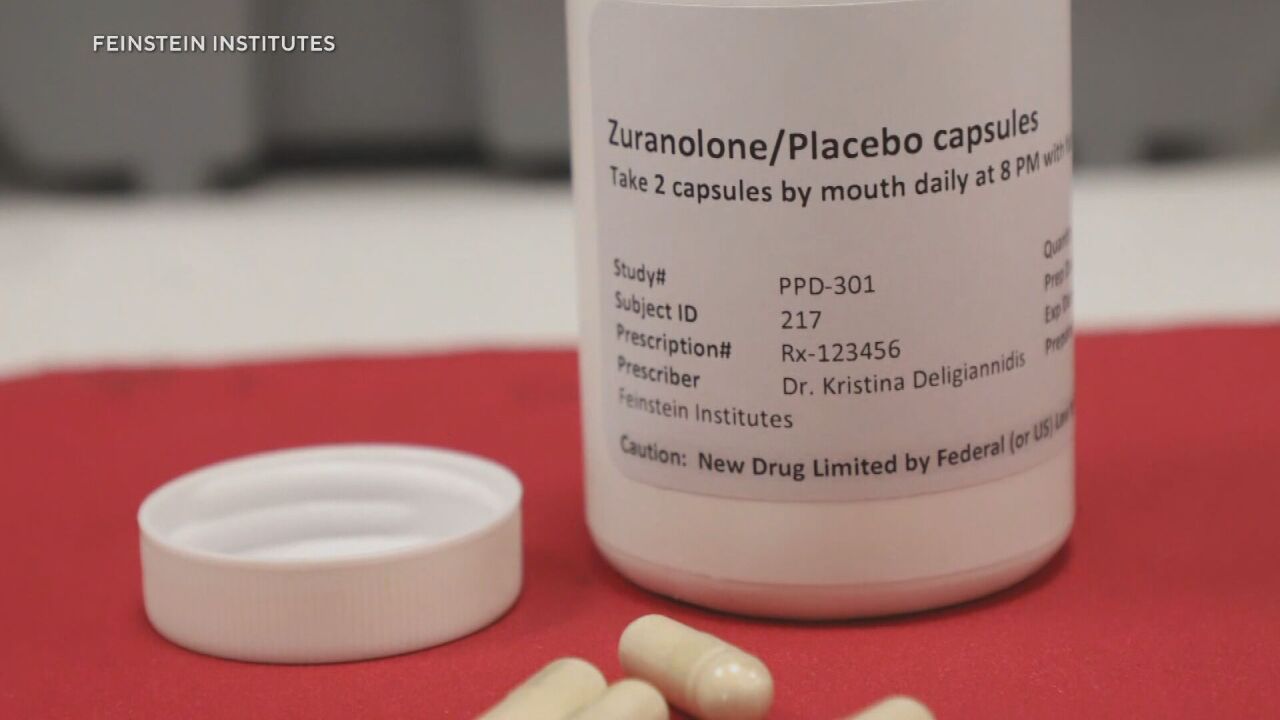
At this point, Richards prescribed zuranolone—the first-ever oral medication specifically designed to treat postpartum depression.
Approved by the Food and Drug Administration (FDA) in August, zuranolone’s availability took several months to materialize.
Many psychiatrists have only recently begun prescribing it as they identify suitable candidates who are open to trying the new drug. They are optimistic about its potential, given that it acts quickly and can be used at home.
Richards mentioned that the woman who was the first of her patients to use zuranolone saw her depressive symptoms begin to improve around three days into the treatment. By day eight, the patient experienced significant improvements and reported no side effects.
“She tells me she feels like she just woke up,” Richards said. “I truly feel like I’m meeting her for the first time. Her husband was in tears, super grateful. Just a major, grand slam success story—which, by the way, we don’t tend to see in psychiatry.”
Postpartum depression can have serious repercussions for both mothers and their children. For mothers, it may increase the risk of suicide, high blood pressure, diabetes, or stroke. Mental illness, suicide, and drug overdoses are leading causes of death within the first year postpartum.
For children, maternal postpartum depression can result in developmental delays, emotional or behavioral issues, and an increased risk of death before the age of one.
Prior to zuranolone, the only available treatment was an intravenous injection approved in 2019. This treatment carries risks such as excessive sedation and sudden loss of consciousness, so it can only be administered in specific treatment centers where patients must stay for 2 1/2 days.
Other women with postpartum depression are typically treated with standard antidepressants, which usually take weeks to become effective. (Zuranolone can be used alongside commonly prescribed antidepressants).
The FDA fast-tracked zuranolone in 2017, a designation for drugs that address serious conditions and fulfill an unmet medical need.
Clinical trials demonstrated that zuranolone could alleviate severe postpartum depression symptoms—such as anxiety, difficulty sleeping, loss of pleasure, low energy, guilt, or social withdrawal—as early as three days into treatment. The medication is taken daily for two weeks, in the evening with a fatty meal.

Doctors believe zuranolone is most appropriate for severe postpartum depression rather than mild cases or “baby blues.” It is considered for patients who struggle with self-care or caring for their babies—those for whom medical intervention could be life-saving.
Despite zuranolone’s potential benefits, some patients are hesitant to use a new drug, citing concerns about side effects or practical barriers.
Zuranolone may cause drowsiness, dizziness, diarrhea, fatigue, and urinary tract infections. Doctors have reported patients experiencing drowsiness or dizziness, though not excessively.
Due to these effects, the medication carries a warning against driving or operating heavy machinery for at least 12 hours after taking it.
Dr. Uruj Kamal Haider, medical director of consultation services at the Massachusetts Child Psychiatry Access Program for Moms, noted that some patients worry about being too tired to care for their babies at night. She recommends having an additional caretaker at home overnight.
“If they have toddlers and they don’t have someone at home to watch the baby or other children at night, that can be very challenging to be on a medication that can make you feel very drowsy,” she said.
Some patients have also declined the medication due to the lack of safety data on breastfeeding. Although a small amount of zuranolone can pass into breast milk, its potential harm is not yet fully studied.
Richards suggests that new mothers might consider discarding their breast milk while taking zuranolone.
Dr. Julia Frew, a psychiatrist at Dartmouth Hitchcock Medical Center, believes that the benefits of breastfeeding may outweigh the risks of medication exposure, particularly since the transfer of other antidepressants through breast milk has not shown significant risks.
“I think it could be a very reasonable choice for someone to continue breastfeeding while they’re taking it,” she said. “Some people may be uncomfortable with that, and they may want to choose to pump and dump.”
Additionally, zuranolone is classified as a Schedule IV controlled substance—similar to Xanax—indicating a low risk of addiction.
“I don’t think we really know the addictive potential. There’s hope that it’s not addictive,” said Dr. Katrina Furey, a clinical instructor in the psychiatry department at Yale School of Medicine.
Haider mentioned that one of her patients completed a 14-day course of zuranolone, with symptom improvement starting by day four.
“The only side effect was drowsiness at night, and that was gone by the morning,” she said. The drowsiness was welcomed by the patient, Haider added, as it helped with sleep.
Frew reported a similar experience with a patient who completed zuranolone treatment this year. This patient, who had chronic depression exacerbated postpartum, found relief with zuranolone after other medications failed.
However, the long-term effectiveness of zuranolone remains uncertain. Trials showed benefits for up to four weeks, but participants were not monitored beyond this period.
“We don’t know yet if people are going to need booster doses down the road,” Furey said.
A ‘cumbersome, clunky’ insurance process
Some psychiatrists have faced difficulties with the insurance approval process for zuranolone.
The medication must be obtained through one of five specialty pharmacies and delivered by mail.
“You cannot pick up zuranolone from your local CVS,” Haider said.
Insurance companies have varying requirements for coverage, with some requiring patients to have tried and failed standard antidepressants first.
“It’s a cumbersome, clunky process,” Richards said, noting that many patients are unable to wait for the process to be streamlined or manage their own deliveries.
“If someone is severely depressed—and that is why you would prescribe zuranolone instead of other options—asking them to wait for this process and engage in it is difficult,” she added.
Nevertheless, psychiatrists are enthusiastic about recommending the drug to their patients.
“I’ve started telling all my patients about it,” Furey said. “Just so they know it’s available and that there is this new option.”