Four individuals in Washington state have tested positive this month for a rare fungal infection that can be fatal.
“It’s the state’s first known outbreak of the fungus, called Candida auris,” said Seattle and King County health officials, “though one locally acquired case was detected there in July. No deaths have been reported.”
The cluster emerges as Candida auris continues its spread across the U.S., with case numbers increasing annually since 2016.
The pathogen is resistant to certain common antifungal drugs and typically affects individuals with weakened immune systems. It is frequently found in hospital patients using catheters, breathing tubes, or feeding tubes.
“Three of the individuals who tested positive in Washington were patients at Kindred Hospital Seattle First Hill,” health officials noted.
“Their cases were identified through a routine screening program designed to detect infections before symptoms appear.”
A fourth patient had previously received care at Kindred but tested positive at a healthcare facility in Snohomish County, according to the Seattle and King County public health department.
The department reported that the first case was notified on January 10, followed by two more on January 22, and a fourth on January 26.
Upon admission to Kindred, all but one patient tested negative for Candida auris, suggesting they acquired the fungus afterward.
“One patient developed an infection,” the health department stated, “indicating the fungus had entered a part of the body where it could cause symptoms, such as the bloodstream, ears, or an open wound.”
The others were colonized with Candida auris, meaning they carried the fungus on their bodies and could potentially spread it to others without showing symptoms. However, colonization still poses a risk of subsequent infection.
Kindred Hospital Seattle First Hill confirmed that all three affected patients are asymptomatic so far and were isolated with enhanced clinical and cleaning precautions to prevent transmission.
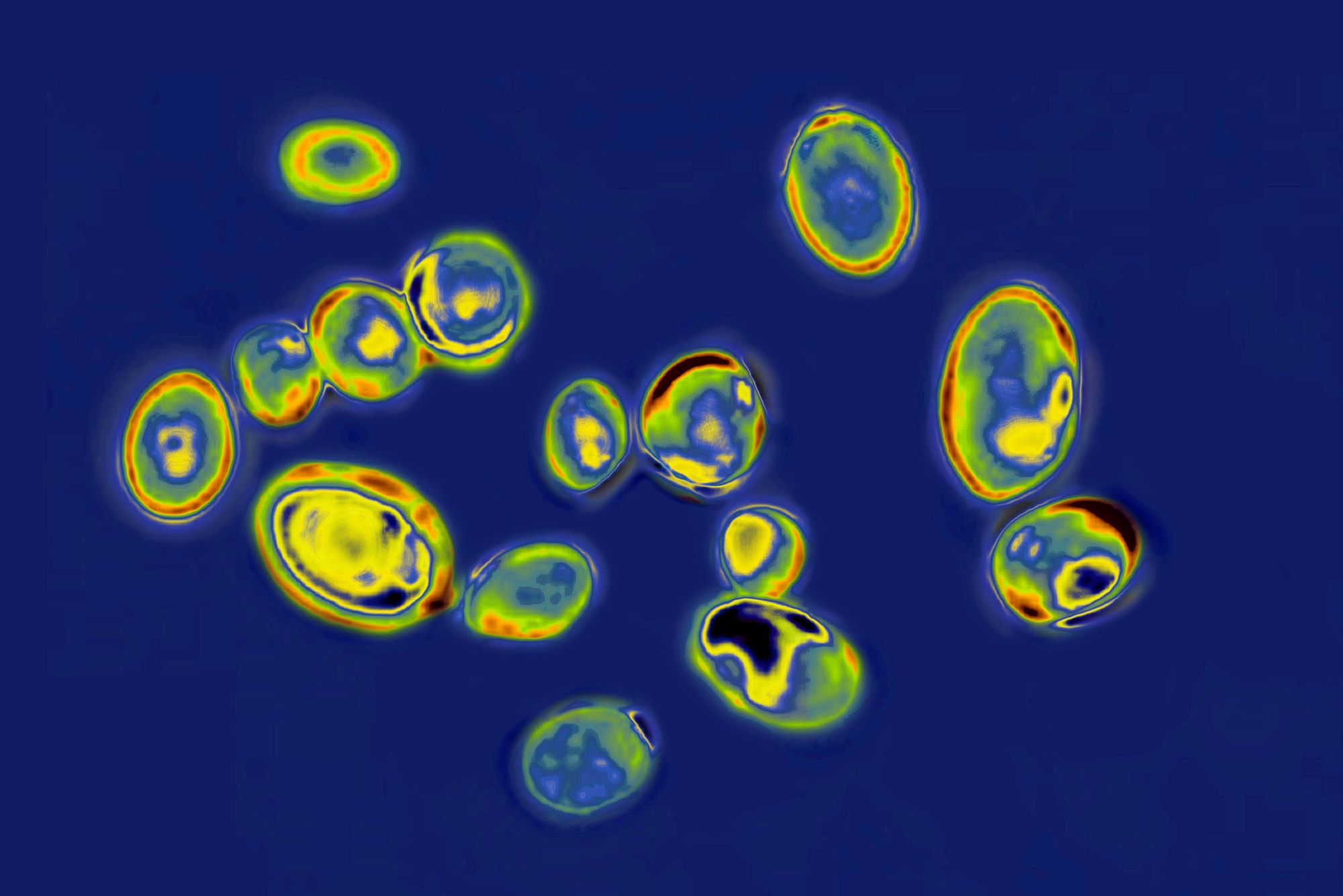
Candida auris was first identified in Japan in 2009 and was later identified in the U.S., prompting the Centers for Disease Control and Prevention (CDC) to request its reporting in 2016. Cases dating back to 2013 were subsequently identified.
Since reporting began, the sharpest increase occurred from 2020 to 2021, with a 94% rise in Candida auris cases.
As of December 2022, the CDC detected the fungus in 36 states. From 2013 to 2022, over 5,600 Candida auris infections were recorded, with an additional 13,000 cases identified through screenings showing no signs of infection.
The CDC attributes the rise of Candida auris to increased screening and inadequate infection control practices in healthcare facilities, exacerbated by staffing shortages and extended patient stays during the COVID-19 pandemic.

“It will definitely spread across the country,” commented Dr. Peter Pappas from the University of Alabama at Birmingham. “The question remains how effectively we can manage it.”
Approximately 90% of Candida auris strains in the U.S. are resistant to the most commonly used antifungal medication for other fungal infections.
While most strains can be treated with drugs from one of three main antifungal classes, some are resistant to all three.
Washington’s initial case was a resident of Pierce County admitted to a local hospital before being transferred to Kindred Hospital Seattle First Hill.
Kindred is the sole facility in Washington conducting universal screening for Candida auris on all new admissions, part of a state initiative launched in 2022.
The screening involves swabbing oily areas like the armpits and groin, where the fungus tends to colonize.
“This marks the first instance where multiple cases have been identified in one setting thanks to the screening program,” remarked Sharon Bogan, a spokesperson for the Seattle and King County health department. “However, it’s challenging to gauge the extent of C. auris circulation.”
Dr. Pappas suggested that the four cases might indicate broader spread in the Seattle area. “By the time it appears in a hospital, it has likely been in the community for some time,” he noted. “The duration of that presence remains unclear.”
He added that distinguishing between infection and colonization is usually straightforward, although there are gray areas. “Those with invasive infections require treatment; otherwise, the consequences could be quite severe.”
The mortality rate for severe Candida auris infections in the U.S. ranges from 30% to 60%, though healthy individuals generally remain unaffected.
Dr. Arturo Casadevall, chair of molecular microbiology and immunology advised that people should find reassurance in active surveillance detecting new cases in their states.
“While it’s unsettling to know it’s present, imagine if we didn’t have surveillance,” he reflected.
He emphasized that the general public need not overly worry about contracting Candida auris just because it’s in the community.
The fungus can spread through direct contact with carriers or contact with contaminated surfaces or objects, with studies showing it can survive on surfaces for at least two weeks.
“Once it enters a hospital, eradicating it becomes challenging,” Casadevall added.