A study published in the journal Science this week has identified a significant and persistent change in certain blood proteins among individuals suffering from long Covid, suggesting that their immune systems remain hyperactive long after the initial infection.
The findings, which could shed light on the root causes of persistent symptoms like fatigue and brain fog, may also pave the way for diagnostic tools and potentially new treatments, experts say.
The research, conducted by scientists who followed 113 Covid patients for up to a year after infection alongside 39 healthy controls, highlighted crucial differences in their blood samples.
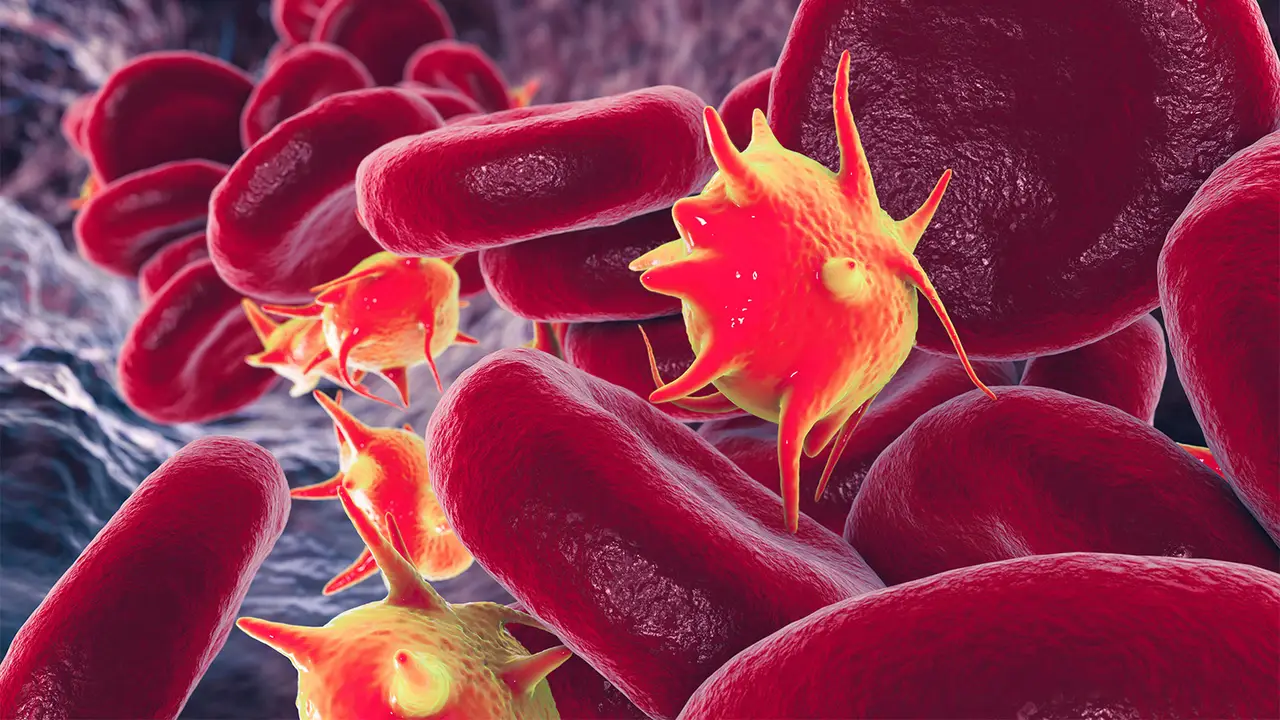
Specifically, proteins linked to the complement system—an essential part of the immune response—showed ongoing activation in long Covid patients. Normally, this system activates to combat infections but should return to a resting state afterward.
Dr. Onur Boyman, a professor of immunology at the University of Zurich and one of the study’s investigators, explained,
“When you have a viral or bacterial infection, the complement system becomes activated and binds to these viruses and bacteria and then eliminates them.”
However, if this activation persists beyond its necessary period, it can begin attacking healthy cells, potentially leading to tissue damage and blood microclots.
Dr. Akiko Iwasaki, a professor at Yale School of Medicine, commented on the study’s significance in understanding the molecular mechanisms behind long Covid symptoms.
She noted that tissue damage and microclots could explain symptoms such as exercise intolerance and cognitive issues seen in long Covid patients.
Dr. Monica Verduzco-Gutierrez, chair of rehabilitation medicine at the University of Texas Health Science Center at San Antonio, emphasized the importance of such mechanistic insights for developing effective treatments.
She highlighted previous studies that also explored different aspects of long Covid, such as the impact of lingering virus remnants on serotonin levels and reduced cortisol levels affecting alertness.
Regarding the potential for diagnostic tests and treatments, Boyman acknowledged the need for further development beyond the study’s sophisticated detection methods.
He stressed the necessity for collaborations with diagnostics companies to streamline testing methods suitable for clinical settings.
Both Iwasaki and Verduzco-Gutierrez expressed optimism about future research directions and the potential for clinical trials of drugs targeting the complement system.
They emphasized the importance of replicating the study’s results and conducting long-term follow-ups on patients to better understand the trajectory of long Covid.
Verduzco-Gutierrez also underscored the need for extended research into patients with long Covid over more extended periods to fully comprehend the condition’s long-term effects.
While the study offers promising insights into long Covid’s underlying mechanisms, its findings are seen as a critical step towards developing targeted therapies and improving patient outcomes.