A significant advancement in Alzheimer’s research has at last provided an answer to a longstanding question that scientists have been pursuing for years.
According to a study published in Science, researchers have uncovered how brain cells perish in individuals developing Alzheimer’s disease.
“This is a very significant and intriguing discovery,” remarked Bart De Strooper, a researcher at the UK Dementia Research Institute, spoke.
“For the first time, we gain insight into how and why neurons die in Alzheimer’s disease. There has been much speculation over the past 30-40 years, but no one has been able to pinpoint the mechanisms.”
Scientists from Belgium and the UK conducted experiments where they transplanted human brain cells into genetically modified mice engineered to produce large quantities of abnormal amyloid.
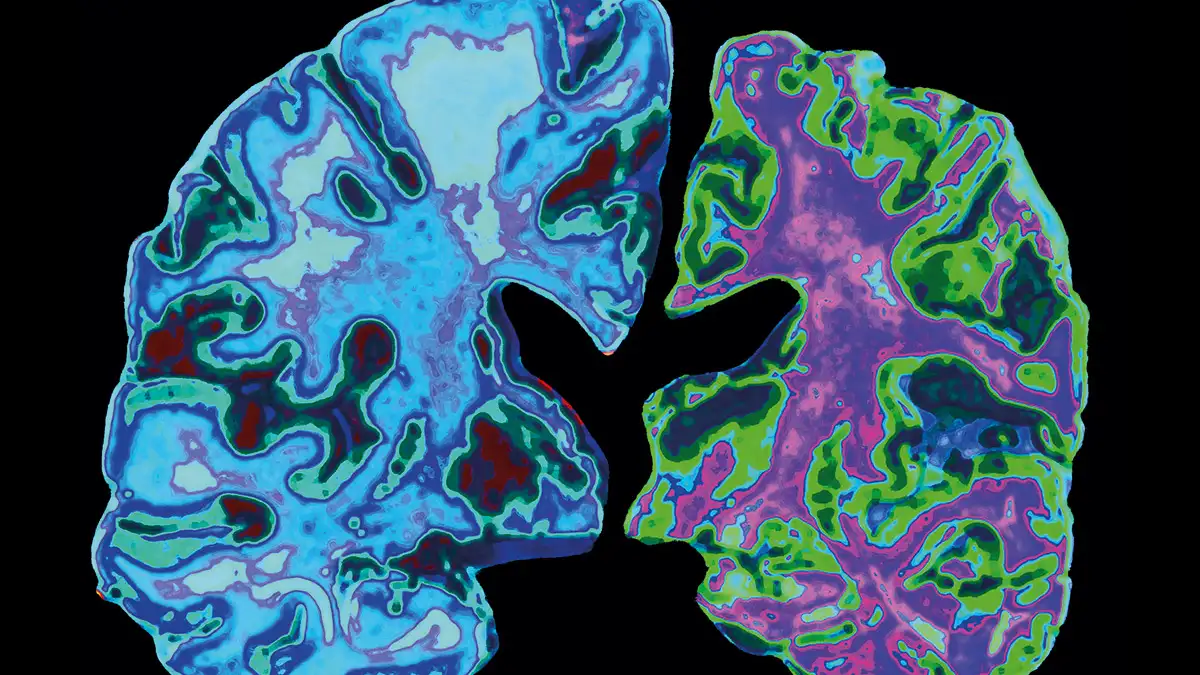
The research determined that the disease progresses through necroptosis—a type of cellular self-destruction. Individuals afflicted with Alzheimer’s undergo neuronal loss and accumulation of abnormal proteins known as amyloid and tau, leading to symptoms such as memory impairment.
“Amyloid is a protein present in our brains and bodies, but in Alzheimer’s disease, it aggregates and forms clumps of various sizes that eventually develop into plaques in the brain,” as described by Alzheimers.org.
Tau, on the other hand, is a protein that “forms insoluble filaments that accumulate as neurofibrillary tangles in Alzheimer’s disease and related tauopathies,” according to the National Library of Medicine.
However, the recent breakthrough has finally elucidated the reasons behind this buildup. The research team now believes that abnormal amyloid initiates its aggregation in the spaces between neurons, triggering brain inflammation that alters internal chemistry.
As tau tangles accrue, brain cells start producing Maternally Expressed Gene 3 (MEG3) molecules, which instigate necroptosis.
With this understanding, researchers were able to enhance the survival of brain cells by obstructing MEG3 production.
De Strooper highlighted that this discovery could open up a “completely new avenue for drug development.”
Experts caution that while these findings represent a significant stride forward, it may take several years before they can be translated into clinical applications.
Tara Spires-Jones, president of the British Neuroscience Association at the University of Edinburgh, told that this research “addresses one of the fundamental gaps in Alzheimer’s research” and emphasized that “these results are fascinating and will be pivotal for future studies.”
However, she emphasized that “many steps are necessary” before this research can translate into tangible benefits for patients grappling with this progressive disease.
