Hispanic dialysis patients face a 40% higher risk of developing a staph bloodstream infection compared to whites, highlighting economic and racial disparities within the U.S. healthcare system, according to new data released Monday by the Centers for Disease Control and Prevention (CDC).
The CDC reported that adults undergoing dialysis for kidney failure were 100 times more likely to contract staph bloodstream infections compared to the general U.S. population.
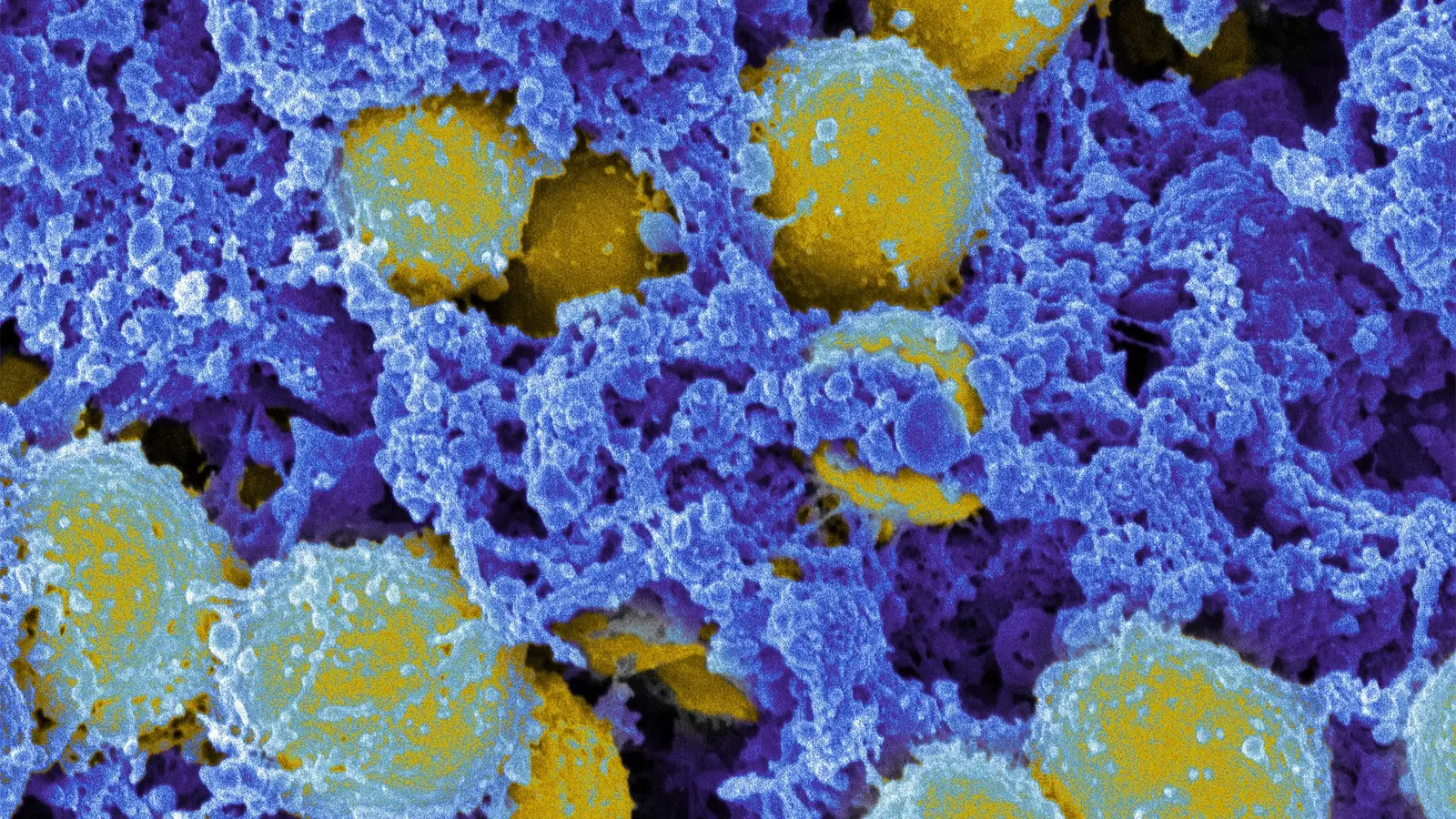
During dialysis, needles and catheters used to connect patients can introduce bacteria like staph into the bloodstream, which can lead to serious and sometimes fatal infections.
“Infections are thought to be the second-leading cause of death in dialysis patients — that’s all infections, not just bloodstream infections,” said Dr. Shannon Novosad, head of the CDC’s dialysis safety team, during a press briefing Monday. “They’re also one of the leading causes of hospitalizations for these patients.”
According to the CDC, over 800,000 people in the U.S. are living with kidney failure, with 70% of them relying on dialysis for treatment.
However, people of color, particularly Black and Hispanic individuals, face a disproportionately higher risk of kidney failure.
They constitute more than half of all dialysis patients, with Black people experiencing a kidney failure rate four times higher and Hispanics twice as high as white individuals, based on CDC data. Black patients account for 33% of all U.S. dialysis patients.

The CDC study, which analyzed data from 2017 to 2020, found that Hispanic and Black patients on dialysis were more likely to contract staph infections compared to their white counterparts. Specifically, Hispanic patients faced a 40% higher risk of staph infection than whites.
“While the unadjusted rate of staph bloodstream infections among Black patients was 23% higher than whites, when adjusted for other factors, they did not have a higher risk,” explained CDC spokesperson Martha Sharan.
“However, it is still important to highlight these high rates because staph bloodstream infections do occur more frequently in Black patients on dialysis, but there are other contributing factors beyond race alone.”
Dr. Novosad noted that a significant number of staph infections among dialysis patients occurred in areas characterized by higher poverty levels, increased household crowding, and lower education levels. Approximately 42% of staph infections were reported in areas with the highest poverty rates.
The CDC’s research focused on data from selected counties in seven states — California, Connecticut, Georgia, Maryland, New York, Tennessee, and Minnesota — over the specified period.
Over the years, bloodstream infections among dialysis patients decreased by 40% from 2014 to 2019 due to enhanced education for staff and patients on infection prevention measures. The use of fistulas and grafts instead of catheters to connect patients to dialysis machines has also contributed to reducing infection risks.
“Preventing staph bloodstream infections begins with early detection of chronic kidney disease to prevent or delay the need for dialysis,” emphasized CDC Chief Medical Officer Dr. Debra Houry.